AbstractThis study was conducted on Korean male high school soccer players who underwent anterior cruciate ligament reconstruction (ACLR) to identify the effects of an accelerated rehabilitation exercise (ARE) program on knee joint isometric strength, thigh circumference, Lysholm score, and active balance agility. We assigned eight test participants each to a physical therapy group (PTG) and an accelerated rehabilitation exercise group (AREG), and compared differences between the groups. Both the PTG and AREG showed significant increases in 30° away and 60° toward isometric strength after treatment. In addition, significant differences were observed in these strength tests between the two groups. Both groups also showed significant increases in thigh circumference, Lysholm score, and active balance agility after treatment, but no significant differences were observed between the two groups. We conclude that the ARE treatment was more effective for improving isometric strength of the knee joint than that of physical therapy, and that an active rehabilitation exercise program after ACLR had positive effects on recovery performance of patients with an ACL injury and their return to the playing field.
INTRODUCTIONSoccer is one of the most popular sports worldwide and more than 200 million professional and amateur soccer players enjoy the sport (Dvorak et al., 2004). Soccer is a sport that anyone can easily participate and have fun while enjoying the benefits of exercise (Lee, 1994). However, competitive soccer involves medium and high intensity contact and collisions, including player-to-player, player-to-ground, player-to-ball, and player-to-goalpost collisions. Most soccer injuries occur to the lower extremities. Ankle injuries account for 16%–29% of all injuries (Junge et al., 2002; Kakavelakis et al., 2003), whereas 7%–36% are knee injuries (Kakavelakis et al., 2003; Söderman et al., 2001). These findings reveal that knee injuries occur predominantly in soccer and injuries of the anterior cruciate ligament (ACL) are the most common in soccer as well as in other sports (Moses et al., 2012). Soccer inherently involves a higher risk of ACL injury than other sports (Alentorn-Geli et al., 2009).
The ACL is one of the four major ligaments that minimize stress on the knee joint and ensures joint stability (Stojanovic and Ostojic, 2012) through resistance against motion caused by anterior tibial translation and internal tibial rotation. ACL injuries often occur due to excessive internal rotation of the femur on the tibia. Although all injuries have a negative impact on player performance, an ACL injury leads to disuse atrophy of the thigh muscles (Takarada et al., 2000), which can reduce hip muscle strength (Elmqvist et al., 1989), and negatively affect performance and recovery time of soccer players. In addition, an ACL injury destabilizes the knee joint, reduces control of nerve roots (Trulsson et al., 2010), decreases active range of motion (ROM) of the joint and increases the possibility of fibrosis and other physical injuries and disabilities (Papandreou et al., 2009). Therefore, a proper rehabilitation program is needed to prevent such secondary dysfunction and disabilities. Conservative treatment is typically used for patients with mild ACL injuries, whereas anterior cruciate ligament reconstruction (ACLR) is performed on those with a severe ACL injury.
Use of a minimally invasive ACLR procedure has enabled quick recovery after surgery, resulting in earlier joint mobility and weight-bearing ability. It has also contributed to increase recovery of performance when combined with an early rehabilitation program immediately after surgery (Cho and Park, 1999). One of the major objectives after ACLR is to recover normal thigh muscle strength (Augustsson et al., 2006) by improving muscle strength and dynamic exercise ability. Thus, various rehabilitation exercise programs can be applied after ACLR. Among them, an accelerated rehabilitation exercise (ARE) program contributes to speed recovery of muscles and prevent complications, including fibrosis of the joint (Wilk et al., 2003). In addition, ARE reduces pain in the knee joint by enabling early weight bearing (Tyler et al., 1998) and can help injured players return to the playing field sooner (Beynnon et al., 2005; Shelbourne and Nitz, 1990). Therefore, we targeted male high school soccer players who underwent ACLR to identify the possible effects of ARE on isometric strength, Lysholm score, and active balance agility. We hypothesized that an ARE program would improve knee joint function in participants who underwent ACLR.
MATERIALS AND METHODSSubjectsThis study was conducted with 16 male high school soccer players who had previously undergone ACLR. The test subjects were diagnosed with a complete ACL rupture, had received an autograft or allograft, and did not have any particular complications or an inflammatory reaction. The test subjects were well informed of the study contents before initiating the rehabilitation or physical therapy program (Ediz et al., 2012; Zalta, 2008) and voluntarily consented to participate.
The participants were divided into an ARE group, who participated in the rehabilitation program (AREG, n=8) and a physical therapy group (PTG) group, who did not participate in the rehabilitation program (PTG, n=8, control). Their physical characteristics are listed in Table 1.
ARE programThe ARE program suggested by Shelbourne and Nitz (1990) was modified and applied as a rehabilitation exercise program carried out in four phases, depending on the presence or absence of pain and the level of muscle improvement of the test subjects. The ARE program started 2 days after surgery and was performed for 2 hr per session, 5 times per week. The objectives of each phase of the ARE program were: Phase 1 was used to relieve inflammation and edema; phase 2 was use to increase ROM; phase 3 was used to boost muscle strength; and phase 4 was used to improve balance ability.
Exercise intensity during each phase was determined after considering the patient’s pain level and compliance with the rehabilitation program. The outline of the ARE program is shown in Table 2.
Lower extremity muscle testThe lower extremity muscle test was performed using the Biodex III (Biodex Medical Systems, Shirley, NY, USA). The subjects sat in the Biodex chair with the hip joint at 90° and the motion axis of the knee joint straight with that of the machine. The trunk, hip, and thigh were fixed with waist and thigh belts.
The medial ankle, its straight upper bone, and a lever were strapped with a belt. The test angles were limited to 0°–90° to prevent any injury during the test. A pre-exercise was done as practice once before the test was conducted.
To test muscle function of the knee joint, maximum away and toward isometric strength of the subjects were measured for 5 sec at knee joint flexion of 30° and 60°, with a 1-min rest between the tests at each angle.
Measurement of femoral circumferenceFemoral circumference was measured using the method suggested by McRae and Esser (2008). After the test subject extended their leg, a point 18 cm from the joint line was marked, and the circumference was measured with a tape.
Dynamic balance ability testDynamic balance ability was measured using the Balance System SD (Biodex Medical Systems). When a moving cursor at the center of a circle displayed on the screen leaned to one side, the subject balanced to maintain the most stable position possible without taking their feet off a footplate. The balance index shows ability to control the unstable circular footplate, which was divided into A, B, C, and D ranges as it moved away from the center of the circle to the perimeter and was sectioned I, II, III, and IV along the X and Y axes. The circular footplate had a 5° incline interval for each range, and the total incline from the stable position to range D was 20°. The A-I, A-II, A-III, A-IV, B-I, B-II, B-III, B-IV, C-I, C-II, C-III, C-IV, D-I, D-II, D-III, and D-IV values were displayed in the pre-/poststate with the inner/outer balance distributions. The overall indices, pre-/postindices, and inner/outer indices were calculated with a computer.
Lysholm score (knee joint function index)The knee joint function index was assessed with Lysholm’s (Lysholm and Gillquist, 1982) scoring criteria. The knee joint function index (or Lysholm index) has a 0–100 point scale, which consists of limp, support, stair-climbing, squatting, instability during walking, running and jumping, pain, swelling, and thigh hypotrophy categories.
Statistical analysisDescriptive data are presented as mean±standard error. A 2 (group: PTG vs AREG) ×2 (time: before and after 12 weeks) repeated-measures analysis of variance for the training and treatment programs was used to assess differences between the conditions. Paired and independent t-tests were carried out to detect differences. A P<0.05 was considered significant. All analyses were performed using IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA).
RESULTSChanges in knee joint isometric force in the PTG and AREGThe 30° away knee joint isometric force increased significantly in the PTG from 162.27%±7.08% before treatment to 194.16% ±8.07% after treatment (P=0.013). The 30° away knee joint isometric force also increased significantly in the AREG from 143.06% ±13.54% to 236.51%±9.7%. A significant group×time interaction was also observed (P<0.001), and a significant difference in the posttreatment 30° away isometric force was observed between the PTG and the AREG (P=0.03).
The 60° toward isometric strength in the PTG increased significantly from 212.83%±17.43% before treatment to 274.3%±19.04% after treatment (P=0.011), and that of the AREG increased from 184.4%±17.67% to 331.38%±27.95% (P=0.004). The 60° toward isometric strength of increased significantly in both groups (PTG, P=0.02; AREG, P<0.001) and between the two groups (P=0.006). These results indicate that the ARE program effectively improved isometric strength of participants who underwent ACLR (Fig. 1).
Influence of PT and ARE on changes in thigh circumference and Lysholm scoreThigh circumference of the PTG increased from 47.22±0.58 to 48.73±0.64 cm (P=0.005), whereas that of the AREG increased from 46.36±0.65 to 48.87±0.84 cm (P=0.002). However, no difference was found between the two groups (Fig. 2).
Influence of PT and ARE on dynamic balanceThe dynamic balance score of the PTG improved significantly from 6.12±0.52 to 3.75±0.43, whereas that of the AREG also improved from 7.32±0.41 to 3.61±0.36. However, no difference was observed between the groups (Fig. 3). These results show that both promoted recovery of dynamic balance in subjects who underwent ACLR.
DISCUSSIONIn this study, we applied either a PT or an ARE program to Korean male high school soccer players who underwent ACLR and examined the effects of both programs on isometric strength, Lysholm score, balance, and thigh circumference. The main finding was that 12 weeks of ARE and PT both had positive impacts on all measured parameters. Notably, the results suggest that ARE could be more effective for improving 30° away and 60° toward isometric strength than those of PT.
Effects of PT and ARE on knee joint isometric strengthKnee joint muscle strength after ACLR tends to decrease on the affected side compared to that on the normal side (Gerber et al., 2009). Edema is likely to occur in knee joints after surgery, which could suppress quadriceps contraction. Prolonged edema can also cause shrinkage of the quadriceps due to the inhibited neuromuscular condition. Previous studies have suggested that 60 mL of edematous fluid can reduce contraction of the quadriceps by up to 50% (Spencer and Hayes, 1984).
Only passive rehabilitation therapies were used in the 1980s, which allowed only 30°–60° of knee joint flexion and banned weight bearing for the first 6 weeks to protect transplanted tissues after ACLR. Later, many studies reported that early passive joint exercise did not impair transplanted muscle tissues, which was later clinically proven (Demaio et al., 1992; Shelbourne and Nitz, 1990). Thus, transplanted muscle tissues were found to play a role as an ACL in the absence of necrotized tissues within 3 weeks after surgery and that an adequate amount of stress to fibroblasts is necessary to facilitate growth of collagenous fibers in transplanted tissues (Hannafin et al., 1995; Rougraff et al., 1993). Isometric exercise is widely used as a rehabilitation exercise for muscle loss and atrophy due to limb fracture. The most important advantage of isometric exercise is that it can be used to assess muscle strength and exercise muscles with limited movement (Wei, 2000). Therefore, isometric exercise is widely used in the early stages of rehabilitation to strengthen the muscles around the knee joint. Isometric exercise, which improves muscle strength using the motion range available depending on the angle of an early unstable injured joint, is a treatment or rehabilitation exercise that is highly stable and provides adequate exercise load to improve muscle strength in patients with exercise injuries using all ROMs (Osternig, 1986). The muscle strength test is mainly used to evaluate recovery after ACLR or to evaluate the effects of a exercise training program (Ageberg et al., 2009).
In this study, both the PT and ARE programs had positive effects on away and toward isometric strength. Karasel et al. (2010) showed a significant difference in knee extensor strength at a 60°/sec angular velocity after applying ARE, whereas Konishi et al. (2012) reported improved extensor muscle strength after closed kinetic channel exercise. Similarly, rehabilitation exercise after ACLR is effective for improving extensor function. We also showed improved away (extension) isometric strength after ARE and PT, indicating that rehabilitation exercise after ACLR could positively affect the extensors. However, the significant change in toward (flexor) isometric tension that we observed was not consistent with results of previous studies. Karasel et al. (2010) reported no differences in flexor muscle strength after ARE, whereas Jang et al. (2011) observed significant changes in extensors but not flexors. This could be ascribed to the compensation mechanism between extensors and flexors, by weakened muscle function, or muscular atrophy of the extensor after ACL injury. In addition, previous studies also observed isokinetic functions, but further studies are needed to assess differences between measurement parameters, but we only evaluated isometric strength within a limited angular range in early-stage injuries.
The PTG and AREG showed significant differences in 30° away and 60° toward isometric strength, indicating that participating in a dynamic rehabilitation program is more suitable for recovering function after ACLR. The results also show that the ARE program was more effective for improving isometric strength of the thigh muscles and knee joint. In addition, because the ability or inability of patients to return to high-intensity sports activities is an indicator to determine the success of ACLR treatment (Kvist, 2004), the ARE applied here could be successful used a rehabilitation exercise program for patients with a limited ROM.
Effects of PT and ARE on thigh circumference and Lysholm scoreThigh muscle atrophy is the most common symptom after knee joint injury due to immobilization after use of a brace. Gerber et al. (1985) reported a 10% decrease in thigh circumference at the quadriceps and a 4% decrease in that of the hamstrings in patients with chronic ACL injuries. Reat and Lintner (1997) also reported that thigh circumference of the affected side decreased 10.8% compared to that of the normal side after ACLR. Itoh et al. (1992) reported that the quadriceps and hamstring can atrophy or weaken substantially if left untreated after an ACL injury.
Arangio et al. (1997) reported that thigh circumference of the affected side that underwent ACLR decreased by 1.8% compared to that of the normal side and that quadriceps area measured by magnetic resonance imaging indicated an 8.6% decrease. As such, an ACL injury reduces thigh circumference and weakens the quadriceps. We observed that thigh circumference increased in both groups, indicating the effectiveness of the programs to prevent muscular atrophy after ACLR. Thigh circumference in the PTG increased by 3.06%, from 47.22±0.58 to 48.73±0.64 cm, whereas that in the AREG increased 5.01% from 46.36±0.65 to 48.87±0.84 cm. This tendency for improvement suggests that a more effective rehabilitation program could be developed if the duration and contents of the program were properly modified before application.
The widely used knee joint function evaluation scales include the Kujala score, the Lysholm score, the Cincinnati knee rating system, and the patellofemoral joint evaluation scale. These methods measure discomfort, pain, and edema. Among them, the Lysholm score consists of items, including limping life, level of support, such as use of braces, stair-climbing, squatting, instability during walking, running, and jumping, pain, swelling, and thigh hypotrophy, and has a 100-point scale (Lysholm and Gillquist, 1982). A score of 95–100 is considered as “excellent,” 84–94, “good,” 65–83, “normal,” and <64, “poor.” This test is widely used in clinical practice and knee joint-related studies (Lysholm and Gillquist, 1982).
Novak et al. (1996) reported that 19 patients who underwent knee arthroscopic surgery for ACLR after ACL injury had average Lysholm scores of 93 points 2 yr after the surgery. Natri et al. (1996) conducted a follow-up observation of 90 patients who underwent ACLR procedure after ACL injury and reported that 76% had Lysholm scores >82 points 3.5 yr after the surgery. In this study, the PTG and the AREG showed significant increases after treatment, although no differences were detected between the groups. The AREG showed a 54% improvement, supporting the argument that more active muscle strengthening exercises during the early stage of rehabilitation is more effective for recovering of muscle and joint functions. An active rehabilitation exercise and treatment program can shorten the recovery time for injured athletes, and accelerate their return to the field (Natri et al., 1996; Novak et al., 1996).
Effects of PT and ARE on active balance abilityThe balance sense of the knee joint is maintained by proprioception from mechanical receptors in ligaments and several other structures to sustain the body balance control mechanism. Shiraishi et al. (1996) conducted a balance test on test subjects by dividing them into an ACLR group, a non-ACLR group, and a normal control group, and reported that the ACLR group showed a lower level of balance ability than that of the normal control group, but a higher level than that of the non-ACLR group. In addition, Mattacola et al. (2002) reported almost no difference on a balance ability test compared to that of the normal control group 18 months after ACLR. Harrison et al. (1994) reported no difference between the ACLR and non-ACLR control group in terms of postural balance control.
Soccer players must have an excellent sense of balance of the foot to control the ball, which is required when they land on the ground after jumping to head the ball. If their balance ability is poor, they are more likely to suffer a sprain or contusion of a knee ligament, so good balance is an important physical requirement for soccer players. Therefore, the balance abilities of soccer players are remarkably better than their ordinary counterparts (Park et al., 2009). We conducted a dynamic balance ability test using a moving ground to evaluate balance control ability of the soccer players. The PTG and AREG showed significant changes between before and after treatments, but no differences between the two groups were observed. The PTG showed only a 41.4% improvement, the AREG presented a 52.1% increase in balance ability, indicating the potential benefits of the ARE.
After applying PT or ARE programs to two groups of male high school soccer players who underwent ACLR procedures after ACL injury, both treatments had positive effects on isometric strength, thigh circumference, Lysolm score, and active balance ability of knee joints. We found that the ARE was particularly more effective for improving 30° away and 60° toward isometric strength. Although no differences were observed between the other parameters, the differences in isometric strength contribute to preventing muscle loss and accelerate recovery from injury. This means that an ARE program is essential for helping injured patients return to the playing field and everyday life and that the benefits of various rehabilitation exercise programs need to be compared and verified to develop a more effective rehabilitation program in the future.
REFERENCESAgeberg E, Roos HP, Silbernagel KG, Thomeé R, Roos EM. Knee extension and flexion muscle power after anterior cruciate ligament reconstruction with patellar tendon graft or hamstring tendons graft: a cross-sectional comparison 3 years post surgery. Knee Surg Sports Traumatol Arthrosc. 2009;17:162–169.
Alentorn-Geli E, Myer GD, Silvers HJ, Samitier G, Romero D, Lázaro-Haro C, Cugat R. Prevention of non-contact anterior cruciate ligament injuries in soccer players. Part 2: a review of prevention programs aimed to modify risk factors and to reduce injury rates. Knee Surg Sports Traumatol Arthrosc. 2009;17:859–879.
Arangio GA, Chen C, Kalady M, Reed JF 3rd. Thigh muscle size and strength after anterior cruciate ligament reconstruction and rehabilitation. J Orthop Sports Phys Ther. 1997;26:238–243.
Augustsson J, Thomeé R, Lindén C, Folkesson M, Tranberg R, Karlsson J. Single-leg hop testing following fatiguing exercise: reliability and biomechanical analysis. Scand J Med Sci Sports. 2006;16:111–120.
Beynnon BD, Uh BS, Johnson RJ, Abate JA, Nichols CE, Fleming BC, Poole AR, Roos H. Rehabilitation after anterior cruciate ligament reconstruction: a prospective, randomized, double-blind comparison of programs administered over 2 different time intervals. Am J Sports Med. 2005;33:347–359.
Cho JH, Park WH. Characteristic analysis of knee joint isokinetic parameters after anterior cruciate ligament reconstruction. Korean J Sports Med. 1999;17:176–187.
DeMaio M, Noyes FR, Mangine RE. Principles for aggressive rehabilitation after reconstruction of the anterior cruciate ligament. Orthopedics. 1992;15:385–392.
Dvorak J, Junge A, Graf-Baumann T, Peterson L. Football is the most popular sport worldwide. Am J Sports Med. 2004;32:1 Suppl. 3S–4S.
Ediz L, Ceylan MF, Turktas U, Yanmis I, Hiz O. A randomized controlled trial of electrostimulation effects on effussion, swelling and pain recovery after anterior cruciate ligament reconstruction: a pilot study. Clin Rehabil. 2012;26:413–422.
Elmqvist LG, Lorentzon R, Johansson C, Långström M, Fagerlund M, Fugl-Meyer AR. Knee extensor muscle function before and after reconstruction of anterior cruciate ligament tear. Scand J Rehabil Med. 1989;21:131–139.
Gerber C, Hoppeler H, Claassen H, Robotti G, Zehnder R, Jakob RP. The lower-extremity musculature in chronic symptomatic instability of the anterior cruciate ligament. J Bone Joint Surg Am. 1985;67:1034–1043.
Gerber JP, Marcus RL, Dibble LE, Greis PE, Burks RT, LaStayo PC. Effects of early progressive eccentric exercise on muscle size and function after anterior cruciate ligament reconstruction: a 1-year follow-up study of a randomized clinical trial. Phys Ther. 2009;89:51–59.
Hannafin JA, Arnoczky SP, Hoonjan A, Torzilli PA. Effect of stress deprivation and cyclic tensile loading on the material and morphologic properties of canine flexor digitorum profundus tendon: an in vitro study. J Orthop Res. 1995;13:907–914.
Harrison EL, Duenkel N, Dunlop R, Russell G. Evaluation of single-leg standing following anterior cruciate ligament surgery and rehabilitation. Phys Ther. 1994;74:245–252.
Itoh H, Ichihashi N, Maruyama T, Kurosaka M, Hirohata K. Weakness of thigh muscles in individuals sustaining anterior cruciate ligament injury. Kobe J Med Sci. 1992;38:93–107.
Jang JW, Kim SS, Kim TS. Effect of 16 weeks functional rehabilitation exercise on knee function recovery in women’s soccer player after anterior cruciate ligament reconstruction. J Sport Leis Stud. 2011;45:863–876.
Junge A, Rösch D, Peterson L, Graf-Baumann T, Dvorak J. Prevention of soccer injuries: a prospective intervention study in youth amateur players. Am J Sports Med. 2002;30:652–659.
Kakavelakis KN, Vlazakis S, Vlahakis I, Charissis G. Soccer injuries in childhood. Scand J Med Sci Sports. 2003;13:175–178.
Karasel S, Akpinar B, Gülbahar S, Baydar M, El O, Pinar H, Tatari H, Karaoğlan O, Akalin E. Clinical and functional outcomes and proprioception after a modified accelerated rehabilitation program following anterior cruciate ligament reconstruction with patellar tendon autograft. Acta Orthop Traumatol Turc. 2010;44:220–228.
Konishi Y, Oda T, Tsukazaki S, Kinugasa R, Fukubayashi T. Relationship between quadriceps femoris muscle volume and muscle torque at least 18 months after anterior cruciate ligament reconstruction. Scand J Med Sci Sports. 2012;22:791–796.
Kvist J. Rehabilitation following anterior cruciate ligament injury: current recommendations for sports participation. Sports Med. 2004;34:269–80.
Lee YS. Prevention program for soccer injuries. Korean J Sports Med. 1994;12:43–53.
Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10:150–154.
Mattacola CG, Perrin DH, Gansneder BM, Gieck JH, Saliba EN, McCue FC 3rd. Strength, functional outcome, and postural stability after anterior cruciate ligament reconstruction. J Athl Train. 2002;37:262–268.
McRae R, Esser M. Practical fracture treatment. 5th ed. Philadelphia: Churchill Livingstone; 2008.
Moses B, Orchard J, Orchard J. Systematic review: annual incidence of ACL injury and surgery in various populations. Res Sports Med. 2012;20:157–179.
Natri A, Järvinen M, Kannus P. Primary repair plus intra-articular iliotibial band augmentation in the treatment of an acute anterior cruciate ligament rupture. A follow-up study of 70 patients. Arch Orthop Trauma Surg. 1996;115:22–27.
Novak PJ, Bach BR Jr, Hager CA. Clinical and functional outcome of anterior cruciate ligament reconstruction in the recreational athlete over the age of 35. Am J Knee Surg. 1996;9:111–116.
Osternig LR. Isokinetic dynamometry: implications for muscle testing and rehabilitation. Exerc Sport Sci Rev. 1986;14:45–80.
Papandreou MG, Billis EV, Antonogiannakis EM, Papaioannou NA. Effect of cross exercise on quadriceps acceleration reaction time and subjective scores (Lysholm questionnaire) following anterior cruciate ligament reconstruction. J Orthop Surg Res. 2009;4:2
Park EK, Chung JW, Jin YS, Chung JS. Association of skill-related fitness with dynamic balance, isokinetic knee strength, and anaerobic power in youth elite soccer player. Korean J Phys Educ. 2009;48:577–584.
Reat JF, Lintner DM. One-versus two-incision ACL reconstruction. A prospective, randomized study. Am J Knee Surg. 1997;10:198–208.
Rougraff B, Shelbourne KD, Gerth PK, Warner J. Arthroscopic and histologic analysis of human patellar tendon autografts used for anterior cruciate ligament reconstruction. Am J Sports Med. 1993;21:277–284.
Shelbourne KD, Nitz P. Accelerated rehabilitation after anterior cruciate ligament reconstruction. Am J Sports Med. 1990;18:292–299.
Shiraishi M, Mizuta H, Kubota K, Otsuka Y, Nagamoto N, Takagi K. Stabilometric assessment in the anterior cruciate ligament-reconstructed knee. Clin J Sport Med. 1996;6:32–39.
Söderman K, Adolphson J, Lorentzon R, Alfredson H. Injuries in adolescent female players in European football: a prospective study over one outdoor soccer season. Scand J Med Sci Sports. 2001;11:299–304.
Spencer JD, Hayes KC, Alexander IJ. Knee joint effusion and quadriceps reflex inhibition in man. Arch Phys Med Rehabil. 1984;65:171–177.
Stojanovic MD, Ostojic SM. Preventing ACL injuries in team-sport athletes: a systematic review of training interventions. Res Sports Med. 2012;20:223–238.
Takarada Y, Takazawa H, Ishii N. Applications of vascular occlusion diminish disuse atrophy of knee extensor muscles. Med Sci Sports Exerc. 2000;32:2035–2039.
Trulsson A, Roos EM, Ageberg E, Garwicz M. Relationships between postural orientation and self reported function, hop performance and muscle power in subjects with anterior cruciate ligament injury. BMC Musculoskelet Disord. 2010;11:143
Tyler TF, McHugh MP, Gleim GW, Nicholas SJ. The effect of immediate weightbearing after anterior cruciate ligament reconstruction. Clin Orthop Relat Res. 1998;357. 141–148.
Wei SH. Dynamic joint and muscle forces during knee isokinetic exercise. Proc Natl Sci Counc Repub China B. 2000;24:161–168.
Fig. 1Effects of 12-week physical therapy (PT) and accelerated rehabilitation exercise (ARE) programs on isometric strength of the knee joint. (A) 30° away and toward in the PT and ARE groups, (B) 60° away and toward in the PT and ARE groups. *Significantly different between pre- and posttreatment at P<0.05. **Significantly different between pre- and posttreatment at P<0.01. ***Significantly different between pre- and posttreatment at P<0.001. #, ##Significantly different between PT group (PTG) and ARE group (AREG) in posttreatment, at P<0.05 and P<0.01, respectively. Pre, pretreatment; Post, posttreatment; BW, body weight. 
Fig. 2Effects of a 12-week physical therapy or accelerated rehabilitation exercise program on thigh circumference and Lysholm score. **Significantly different between pre- and posttreatment at P<0.01. Pre, pretreatment; Post, posttreatment; PTG, physical therapy group; AREG, accelerated rehabilitation exercise group. 
Fig. 3Effect of a 12-week physical therapy or an accelerated rehabilitation exercise program on active balance agility. ***Significantly different between pre- and posttreatment at P<0.001. Pre, pretreatment; Post, posttreatment; PTG, physical therapy group; AREG, accelerated rehabilitation exercise group. 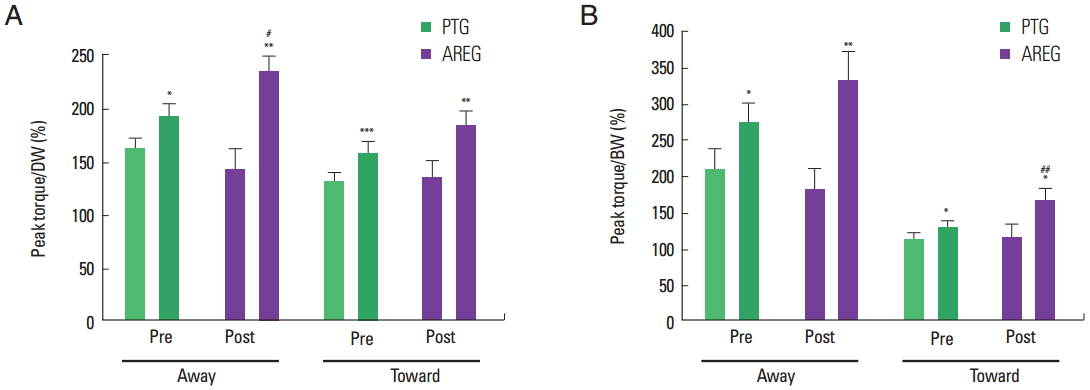
Table 1General characteristics of subjects
Table 2Accelerated rehabilitation exercise programs |
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||