INTRODUCTION
Total hip arthroplasty (THA) is performed surgically in cases such as femoral fracture (Guyen, 2019), arthritis (Gademan et al., 2016), developmental dysplasia of the hip (Greber et al., 2017), and osteonecrosis (Kuroda et al., 2021). Most patients experience disabilities such as muscle weakness, balance and gait disorders with severe pain before THA (Hunter and Bierma-Zeinstra, 2019; Picorelli et al., 2018; Rasch et al., 2007). After THA, patients experience reduced pain and improved hip joint function and quality of life (Bahl et al., 2018; Nguyen et al., 2019; Shan et al., 2014). However, some patients may experience balance problems due to decreased proprioception after THA (Wareńczak and Lisiński, 2019). Balance problems have been reported to persist for up to 5 years after THA (Labanca et al., 2021), and they can also contribute to an increased risk of falls and decreased quality of life (Bobić Lucić and Grazio, 2018; Lo et al., 2019). As such, balance disorders can occur both before and after THA, and in some cases, patients may require revision surgery if they experience falls after THA (Lands et al., 2021).
Exercise therapy must be executed in a systematic manner based on exercise prescription. One of the typical principles in exercise prescription is the FITT principle. FITT stands for frequency, intensity, time, and type (Garber et al., 2011). Exercise therapy can lead to side effects if performed incorrectly (Niemeijer et al., 2020). Therefore, it is important to perform exercise therapy in a systematic manner.
Following THA, patients typically undergo exercise therapy as part of the rehabilitation process (Bandholm and Kehlet, 2012). Physical therapists frequently employ exercise therapy, including gait training, range of motion exercises, and balance training after THA (Peter et al., 2014). Exercise therapy has shown to reduce pain and improve physical activity levels in patients (Wu et al., 2019). A systematic review and meta-analysis reported the effectiveness of exercise therapy on muscle strength and gait after THA (Chen et al., 2021; Coulter et al., 2013). However, the evidence regarding the effects of exercise therapy on balance was found to be insufficient in the systematic review.
Previous systematic reviews have examined the role of exercise therapy on balance before and after THA and total knee arthroplasty (Domínguez-Navarro et al., 2018). However, only one study included in the analysis investigated the intervention after THA. Additionally, other systematic reviews conducted to evaluate balance after THA emphasized the need for further research on interventions (Di Laura Frattura et al., 2022; Labanca et al., 2021). Therefore, the purpose of this systematic review and meta-analysis is to analyze the effects of exercise therapy on the balance and gait of patients after THA.
MATERIALS AND METHODS
Protocol and registration
This systematic review and meta-analysis were registered in the PROSPERO (no. CRD42022343300). We followed the preferred reporting items for systematic reviews and meta-analysis (PRISMA) guidelines while reporting this study (Page et al., 2021).
Eligibility criteria
The selection criteria for this study were based on the PICO-study design criteria, which includes patient (P: patients after THA or total hip replacement), intervention (I: exercise therapy), comparison (C: control and other interventions), outcome (O: balance, gait), and study design (randomized controlled study). The reporting characteristics were language (English) and publication status (journal), and the year of publication was not limited.
Search strategy
Articles relevant to the research question were identified from PubMed, Cochrane Library, Embase, and CINAHL. Each database was searched from their inception until June 30, 2022. For PubMed searches, the search terms are ((“Arthroplasty, Replacement, Hip” [Mesh]) OR (“Arthroplasty, Replacement, Hip”[TIAB]) OR (“total hip arthroplasty”[TIAB]) OR (“total hip replacement”[TIAB])) AND ((“Rehabilitation”[Mesh]) OR (“Exercise Therapy”[Mesh]) OR (“Rehabilitation”[TIAB]) OR (“Exercise Therapy”[TIAB])).
Study selection
Duplicate studies were identified and excluded using a bibliography management software (EndNote X9, Clarivate Analytics, London, UK). Two reviewers independently assessed eligible studies by screening their titles and abstracts and checking the full-text of the selected articles. In cases of disagreement, a consensus was sought between the reviewers.
Data extraction and synthesis
Data extraction and synthesis were performed independently by two reviewers using a standardized data collection form for the following data: year of publication, first author’s name, country, patient characteristics, intervention method, outcomes, and results. In cases of disagreement, a consensus was sought between the reviewers.
Risk of bias assessment
The Cochrane risk of bias assessment tool (RoB 2.0) was used to evaluate the risk of bias in the articles selected for this study. This tool was developed to assess the risk of bias in randomized controlled trials (Sterne et al., 2019).
Statistical analyses
The meta-analysis was performed using a R program (The R Project for Statistical Computing version 4.0.3, ‘meta’ package; R Foundation for Statistical Computing, Vienna, Austria). In the meta-analysis, when comparing the outcomes measured on different scales, the standardized mean difference (SMD) with 95% confidence intervals (CIs) was used. The subgroup analysis was performed according to the duration of intervention in terms of the overall effect size on balance and gait. Reporting bias refers to the convenience of publishing research results; hence, a visual analysis was performed.
RESULTS
Search results
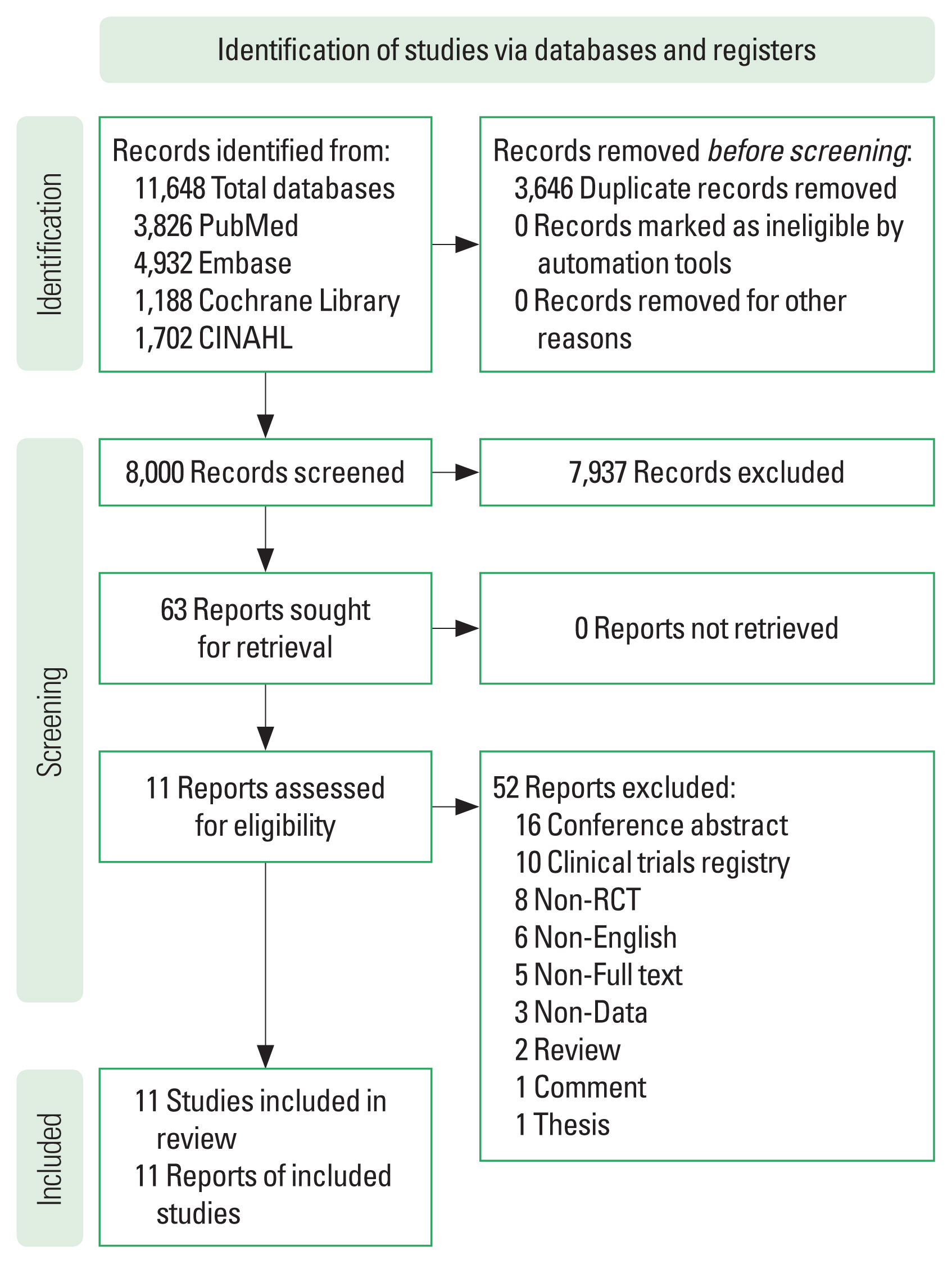
A PRISMA study selection flow chart is shown in Fig. 1. In total, 11,648 studies were identified, with 8,000 remaining after duplicates were removed. Next, 7,937 studies were excluded after screening the titles and abstracts, leaving 63 articles for full-text review. Of the 63 articles, 52 were excluded after a full-text review, leaving 11 articles for risk of bias assessment and meta-analysis.
Characteristics of the studies
Table 1 presents the characteristics of the selected studies included in this analysis. 11 randomized controlled trials were included and the publication years ranged from 2003 to 2022. The number of study participants ranged from 20 to 79. The included studies were classified according to duration of intervention. A study involving duration of intervention with less than 8 weeks was classified as the short-term group, another study involving duration of intervention with 8 weeks or longer as the long-term group.
Risk of bias assessment
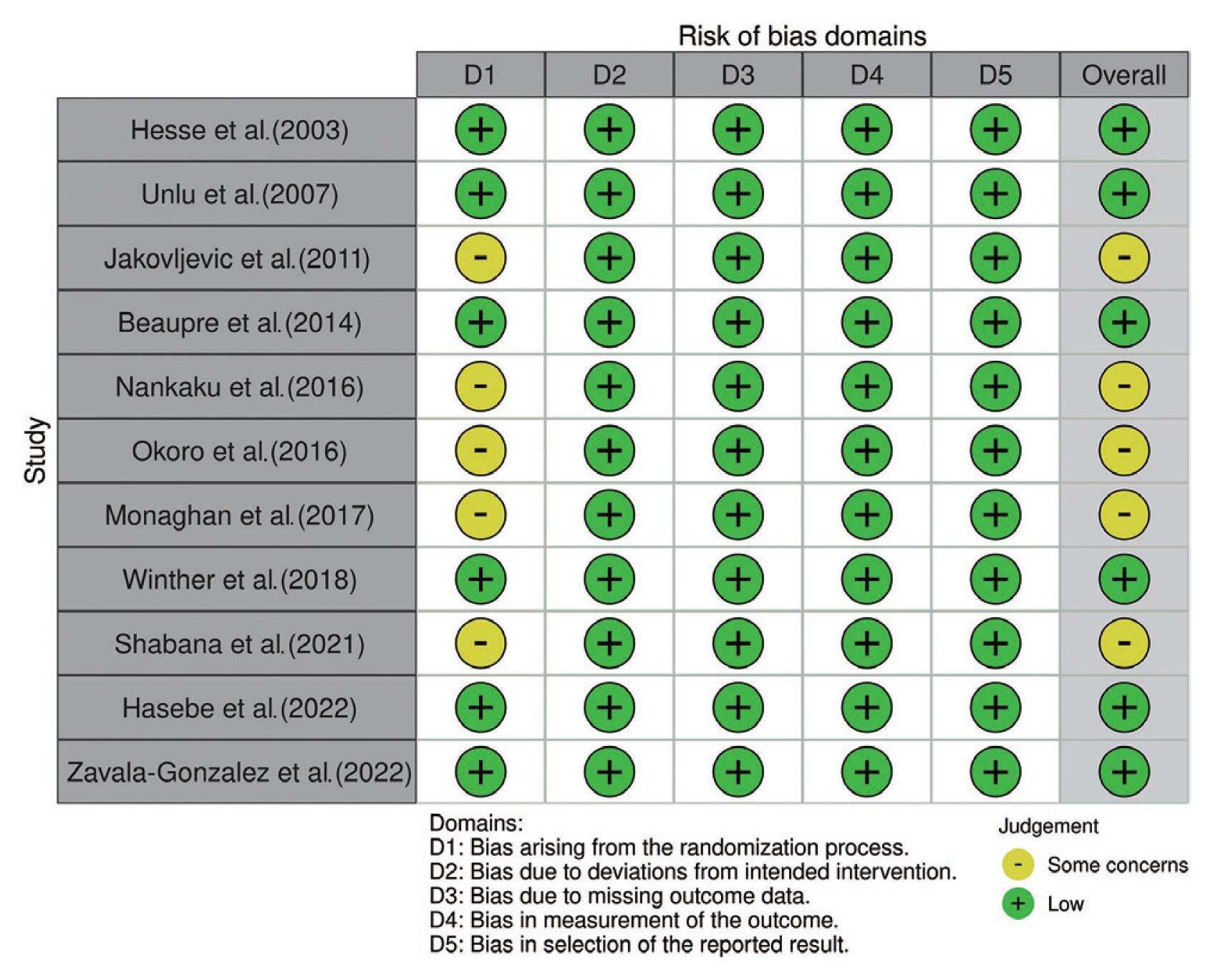
The risks of bias in the 11 individual studies included in this analysis are illustrated in Fig. 2. Regarding bias arising from the randomization process, 6 studies were rated as low-risk, and 5 studies indicated some concern. Regarding bias due to deviations from the intended interventions, bias due to missing outcome data, bias in outcome measurement, and selection bias, 11 studies were rated as low-risk.
Overall effect size of exercise therapy on balance after total hip arthroplasty
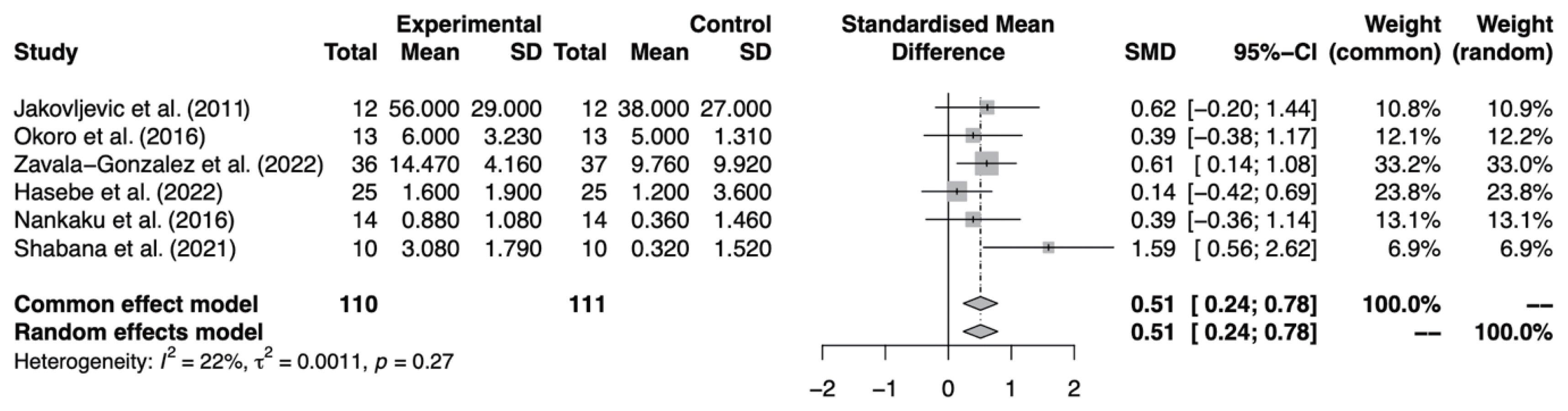
The balance analysis was based on 6 studies (Fig. 3). Significant differences were observed in the comparison of exercise therapy with the control group (SMD, 0.51; 95% CI, 0.24–0.78; I2=22%).
Overall effect size of exercise therapy on gait after total hip arthroplasty
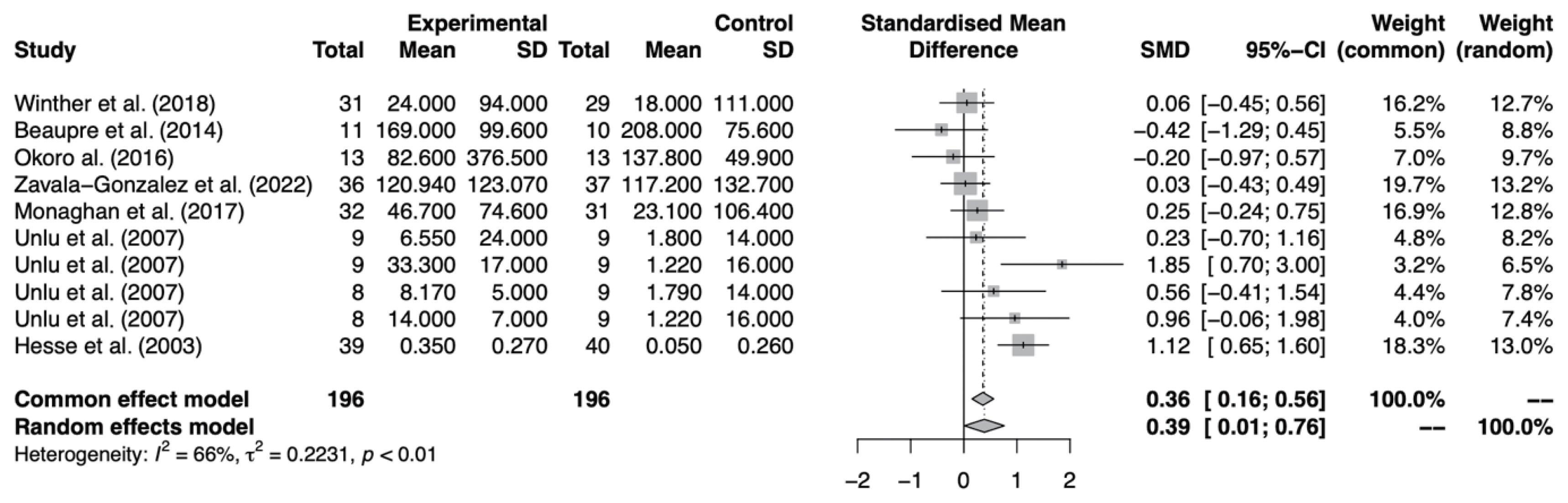
The gait analysis was based on 7 studies (Fig. 4). Significant differences were observed in the comparison of exercise therapy with the control group (SMD, 0.39; 95% CI, 0.01–0.76; I2=66%).
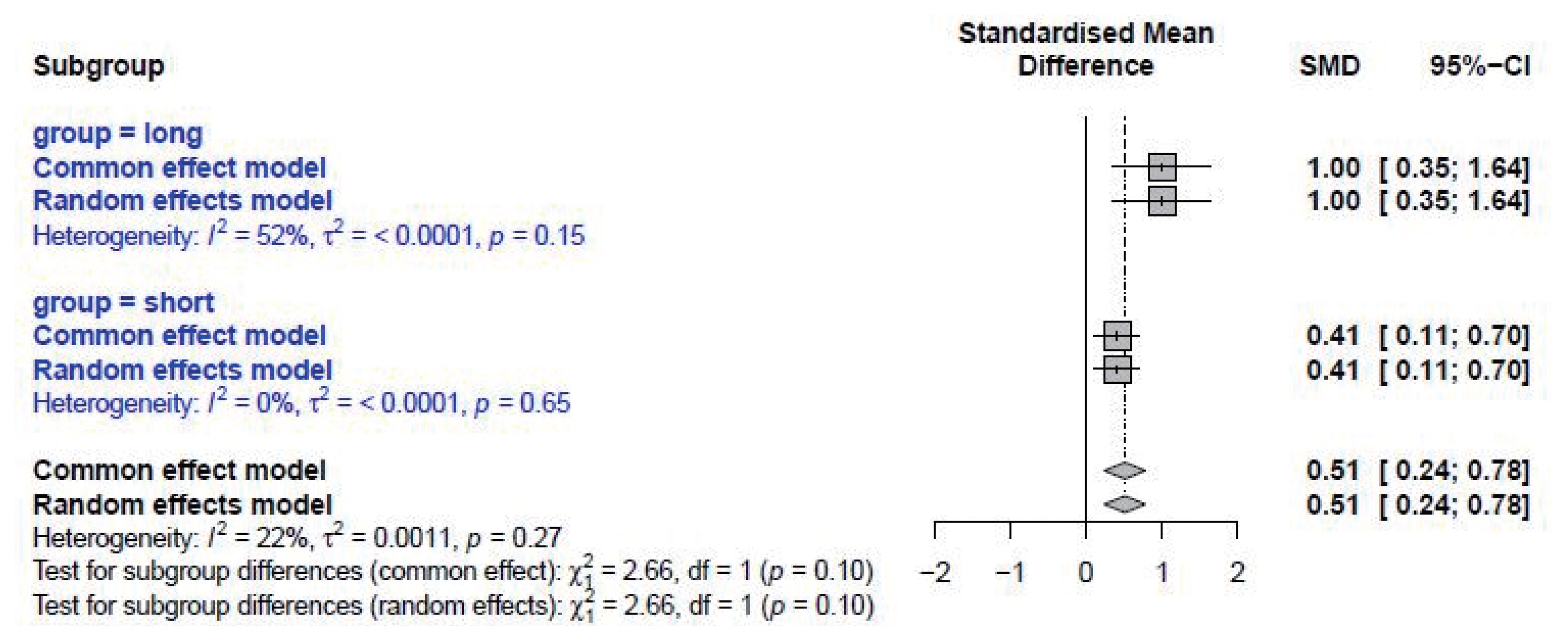
Effect size of exercise therapy on balance according to the duration of intervention
Subgroup analysis was based on the duration of intervention with short term and long term (Fig. 5). Significant differences were observed in the short-term group (SMD, 0.41; 95% CI, 0.11–0.70; I2=0%). Furthermore, significant differences were observed in the long-term group (SMD, 1.00; 95% CI, 0.35 –1.64; I2=52%).
Effect size of exercise therapy on gait according to the duration of intervention
Subgroup analysis was based on the duration of intervention with short term and long term (Fig. 6). Significant differences were observed in the short-term group (SMD, 0.53; 95% CI, 0.12–0.93; I2=67%). However, no significant differences were observed in the long-term group (SMD, −0.13; 95% CI, −0.91 to 0.64; I2=0%).
Publication bias analysis of the effect of exercise therapy on patients after total hip arthroplasty
The visual analysis of publication bias in this study is as follows. As the graph is asymmetrical, it appears that publication bias exists (Fig. 7). The included studies are mainly distributed at the bottom of the graph, indicating that the sample sizes are small.
DISCUSSION
The purpose of this study was to conduct a systematic review and meta-analysis of the effects of exercise therapy on the balance and gait of patients after THA. According to the results of this study, exercise therapy was found to be effective in improving both balance and gait.
There have been studies reporting balance impairment in patients after THA (Queen and Schmitt, 2021; Truszczyńska-Baszak et al., 2021; Wareńczak and Lisiński, 2020). However, there lack of systematic reviews and meta-analyses evaluating patients’ balance after exercise therapy. The study found medium and small effect sizes for the effects on balance and gait. The relatively small effect sizes are thought to be due to the heterogeneity of exercise therapies, which were not independent interventions, resulting in medium (balance) and small (gait) effect sizes. All 11 studies included in this study performed additional exercise therapy after the intervention, the same as the control group. Since the intervention was performed on the patient after the surgery, there was also an effect of the intervention in the control group. The 11 studies included in this study used various exercise therapies ranging from strength training to aquatic exercise. Previous studies have reported that various interventions are used in exercise therapy for patients after THA (Di Monaco and Castiglioni, 2013; Wijnen et al., 2018). Therefore, it is believed that there may be heterogeneity between exercise therapies. Nevertheless, this study found that exercise therapy was effective in balance and gait in patients after THA. Balance disorders are associated with gait and falls (Sihvonen et al., 2009). If a patient experiences a fall after THA, additional fractures or dislocations may occur, leading to the need for revision surgery (Lands et al., 2021). Therefore, it is recommended for patients or rehabilitation specialists to perform systematic exercise therapy based on principles such as FITT in order to prevent falls.
This study conducted subgroup analysis based on the duration of intervention. Balance was significant in both the short and long term. However, gait was significant in the short term but not in the long term. Previous meta-analyses also showed significant results in gait speed (Wu et al., 2019). Studies included in the short term assessed gait using gait speed and 6-min walking test. The long term only included 6-min walking test. Previous studies reported that strength training did not have an impact on gait in the long term, as 6-min walking test assesses cardiopulmonary endurance during gait (Beaupre et al., 2014; Winther et al., 2018). It is important to consider which tools are used to assess gait.
This study has several limitations. The first limitation is that only English literature was included. The second limitation is that studies without sufficient data were not included. Future research that addresses these limitations will be necessary.
CONCLUSION
This systematic review and meta-analysis confirmed that exercise therapy could improve balance and gait in patients after THA. Rehabilitation specialists recommend that exercise therapy be included in rehabilitation programs to improve balance and gait in patients after THA. Further research is needed in the future, including more studies and a network meta-analysis that analyzes the effect size of each exercise.