Effect of pelvic belt on the perception of difficulty and muscle activity during active straight leg raising test in pain-free subjects
Article information
Abstract
A pelvic belt decreases patient-reported perception of difficulty during the active straight leg raising (ASLR) test in individuals with pelvic girdle pain. However, the influence of a pelvic belt on the perception of difficulty during ASLR was not investigated in pain-free subjects. Therefore, this influence excluding the impact of pain is not clear. This paper aimed to clarify the effect of a pelvic belt on the perception of difficulty and muscle activity during ASLR performance in the subjective heavier side leg in pain-free subjects. Twenty pain-free female subjects participated. ASLR using the subjective heavier side leg was performed under two conditions: without and with a pelvic belt. Muscle activation of the external oblique, internal oblique, rectus abdominis, rectus femoris, and biceps femoris was measured during ASLR using a surface electromyograph. Difference in perceived difficulty in performing ASLR with and without a belt was assessed. In total, 80% of subjects had decreased perception of difficulty using a pelvic belt during ASLR. For ASLR performed with a pelvic belt, muscle activity significantly decreased in the contralateral rectus abdominis, ipsilateral external oblique, and bilateral internal oblique (P<0.05), while it significantly increased in the contralateral biceps femoris (P<0.05). There were no significant differences in muscle activity of the ipsilateral rectus abdominis, contralateral external oblique, and ipsilateral rectus femoris between the two conditions (P>0.05). In conclusion, using a pelvic belt can decrease the perception of difficulty during ASLR, and the pelvic belt may improve impairment of load transfer between the trunk and pelvis.
INTRODUCTION
The stability of the lumbopelvic region and effective load transfer is obtained by the neural control subsystem, the active subsystem, and the passive subsystem (Panjabi, 1992). The sacroiliac joint stability depends on specific anatomical features, termed form closure and on muscles and ligaments crossing the sacroiliac joint, termed force closure (Snijders et al., 1993; Vleeming et al., 1990). Instability of the lumbopelvic region has relevance to lumbopelvic pain (Panjabi, 2003), and groin pain (Jansen et al., 2009). Pregnancy-related lumbopelvic pain and sports-related groin pain had a prevalence of 22%–90% (Albert et al., 2001; Nwuga, 1982) and 8%–22% (Gabbe et al., 2010; Paajanen et al., 2011), respectively.
The active straight leg raising (ASLR) test is used for the assessment of lumbopelvic stability of patients with lumbopelvic pain and groin pain (Sawle et al., 2019), muscle recruitment pattern, excessive lumbopelvic movement (Bruno et al., 2014), and patient-reported perception of difficulty (Bruno et al., 2014; Mens et al., 2002). Previous research has suggested that patients with chronic groin pain show delayed activation of the transversus abdominal muscle (Cowan et al., 2004), patients with pregnancy-related lower back pain and pelvic pain display overactivity of external oblique (EO) (de Groot et al., 2008), and patients with chronic pelvic girdle pain display a bracing strategy by bilateral tonic activation of the internal oblique (IO) and EO, unlike healthy subjects (Beales et al., 2009). In addition, it has been reported that patient-reported perception of difficulty during ASLR is involved in disease severity in patients with lower back pain (Bruno et al., 2014; Mens et al., 2002).
A pelvic belt is used in individuals with instability of the sacroiliac joint and lumbopelvic region. A pelvic belt has been reported to increase sacroiliac joint stiffness (Damen et al., 2002) and to decrease pain (Arumugam et al., 2012; Jansen et al., 2009). In addition, a pelvic belt has been reported to decrease patient-reported perception of difficulty during ASLR in people with pelvic girdle pain (Mellin, 1990; Mens et al., 1999). However, the influence of a pelvic belt on perception of difficulty during ASLR was not investigated in pain-free subjects. Therefore, the influence of a pelvic belt on perception of difficulty during ASLR excluding the influence of pain is not clear.
A pelvic belt has been reported to change the muscle recruitment pattern in individuals with pelvic girdle pain (Beales et al., 2010). In addition, Hu et al. (2010) reported that in healthy subjects, activity of the lateral abdominal muscle decreased by using a pelvic belt during ASLR. However, the influence of a pelvic belt on muscle activity was not investigated in ASLR performance in the leg of the subjective heavier side of pain-free subjects. The feeling “heavy” during ASLR has been reported to indicate impairment of load transfer between the trunk and pelvis (Mens et al., 2010). Therefore, the influence of a pelvic belt on muscle activity during ASLR performance in the leg of the subjective heavier side is not clear. The aim of this study is to clarify the effect of a pelvic belt on the perception of difficulty and on muscle activity during ASLR performance in the leg of the subjective heavier side in pain-free subjects.
MATERIALS AND METHODS
Participants
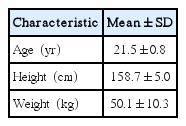
Twenty pain-free female subjects participated in this study. The exclusion criteria were pregnancy, and past or present musculoskeletal, neurological, psychological, or cardiopulmonary disease. People who felt no difference in heaviness between both feet during ASLR were also excluded from the study. Before data collection, all the procedures were explained to the participants, and they signed an informed consent form. This study was approved by the Kawasaki University of Medical Welfare Research Ethics Committee (approval number: 17-099).
Procedure
Initially, the subjects performed ASLR on the left and right legs and decided which leg felt the heaviest. Subjects performed the ASLR using the leg of the subjective heavier side in this study. ASLR was performed under two conditions: without a pelvic belt and with a pelvic belt. The pelvic belt (COM-PRESSOR, OPTP Co., Minneapolis, MN, USA), which consists of four elastic bands and a main body belt, was placed below the anterior superior iliac spine (ASIS) (Jung et al., 2013). For performing ASLR, subjects were asked to lie supine on a treatment bed with the lower extremity, pelvis, and trunk in a straight line. Both arms were placed on their chest to prevent pushing against the bed. The subjects raised their leg of the subjective heavier side without and with a pelvic belt until their leg touched the indicating bar, which was placed 20 cm above the bed while maintaining the knee in extended position (Fig. 1). This position was hold for 5 sec. ASLR without and with a pelvic belt was repeated 2 times each. There was a 1-min rest between each trial. The order of measurements was randomly assigned.
Electromyography
Surface electromyography (EMG) (Vital Recorder; Kissei Comtec Co., Matsumoto, Japan) with a 1,000-Hz sampling frequency was used to measure muscle activities. The following muscles were measured: the bilateral rectus abdominis (RA: about 2–3 cm lateral to the umbilical region), the bilateral EO (15 cm lateral to the umbilicus), the bilateral IO (2 cm medial and inferior to the ASIS), rectus femoris (RF: at 50% on the line from the superior part of the patella to the ASIS) on the leg raising side, the biceps femoris (BF: at 50% on the line between the lateral epicondyle of the tibia and the ischial tuberosity) on the non-leg raising side. The reference electrode was placed on the patella of the leg raising side. Bipolar surface electrodes (P-00-S; Ambu Inc., Ballerup, Denmark) were applied after successful skin preparation using sanding and alcohol. Each pair of electrodes was attached 2.5 cm apart and aligned parallel to muscle fibers. All EMG data were processed through a bandpass filter (15–500 Hz) and full-wave rectified. The average EMG amplitudes of the medial 3 sec of the total 5-sec duration of ASLR were determined. Mean amplitudes of the maximal voluntary isometric contraction (MVIC) were used for normalizing the average EMG amplitudes recorded during ASLR (%MVIC). The MVIC values of each muscle were performed in the manual muscle testing positions.
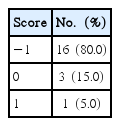
Subjects’ scores (perception of difficulty)
Following the completion of each test, each subject was asked to score difference in her perceived difficulty in performing ASLR with a belt compared with performing ASLR without a belt using the following three-point scale: −1=ASLR with a pelvic belt reduced the difficulty compared to ASLR without a pelvic belt; 0=ASLR with a pelvic belt and ASLR without a pelvic belt had the same perception of difficulty; 1=ASLR with a pelvic belt increased the difficulty compared to ASLR without a pelvic belt.
Statistical analysis
The Shapiro–Wilk test was used to confirm whether muscle activity data approximated a normal distribution. Values of muscle activity during ASLR were not normally distributed; therefore, the Wilcoxon signed-rank test was used to detect differences in muscle activity between ASLR without and with a pelvic belt. The χ2 goodness-of-fit test was used to evaluate the differences in the rate of each score of perceived difficulty. IBM SPSS Statistics ver. 22.0 (IBM Co., Armonk, NY, USA) was used for statistical analyses. Significance was set as α=0.05.
RESULTS
Table 1 shows the physical characteristics of the participants. The scores indicating differences in their perceived difficulty in performing ASLR with a belt compared with performing ASLR without a belt are shown in Table 2. In total, 80% of subjects had decreased perception of difficulty while using a pelvic belt during ASLR, and there was a significant difference in the rate of each score of perceived difficulty (P<0.001).
Result of scores indicating difference in the perceived difficulty in performing ASLR by person with a belt compared with performing ASLR without a belt
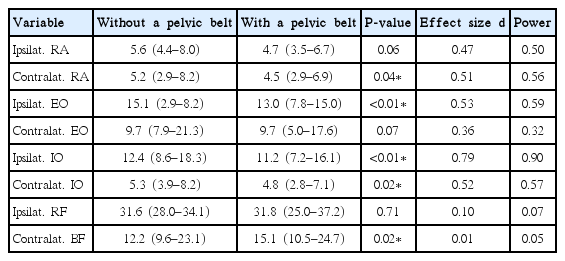
The activity of each muscle during ASLR without and with a pelvic belt is shown in Table 3. For ASLR performed with a pelvic belt, the muscle activity significantly decreased in the contralateral RA, ipsilateral EO, and bilateral IO (P<0.05) while the muscle activity significantly increased in the contralateral BF (P<0.05). There were no significant differences in muscle activity of ipsilateral RA, contralateral EO, and ipsilateral RF between the two conditions (P>0.05).
DISCUSSION
The goal of this study was to clarify the effect of a pelvic belt on the perception of difficulty and on muscle activity during ASLR performance in the leg of the subjective heavier side in pain-free subjects. In this study, the pelvic belt significantly decreased activity in the contralateral RA, ipsilateral EO, and bilateral IO during ASLR performance in the leg of the subjective heavier side, while the muscle activity significantly increased in the contralateral BF. This result resembles that of a previous study that investigated the muscle activity in healthy subjects during ASLR (Hu et al., 2012). The IO and EO activity have been theorized to act as force closure and increases the stability of the lumbopelvic region (Hu et al., 2012). Pelvic belt has been reported to increase sacroiliac joint stiffness (Damen et al., 2002). Therefore, we propose that the activity of the IO and EO, which act as force closure, decreased during ASLR using a pelvic belt because the pelvic belt substitutes as the force closure. In addition, for the ASLR, the mechanical effect of hip flexor muscles is to pull the ilium forward (Hu et al., 2010; Hu et al., 2012). Abdominal wall muscles and contralateral BF act to prevent anterior rotation of the pelvis and to maintain a neutral position of the pelvis against the anterior rotation of the pelvis during ASLR (Hu et al., 2010; Hu et al., 2012). It is possible that with a pelvic belt, because the contralateral RA, ipsilateral EO, and bilateral IO were less active, the contralateral BF was more active to prevent anterior rotation of the pelvis.
In this study, 80% of subjects showed decreased perception of difficulty by using a pelvic belt during ASLR performance in the leg of the subjective heavier side. Mens et al. (1999) have shown a decreased perception of difficulty during ASLR by using a pelvic belt in individuals with pelvic girdle pain. In this report (Mens et al., 1999), because subjects were patients with pelvic girdle pain, decreased pain and increased stability of sacroiliac joint by using a pelvic belt might have been decreasing the perception of difficulty during ASLR. In this study, however, since the subjects were pain-free, decreased perception of difficulty during ASLR was not caused by a change in the degree of pain. We believe that change in the muscle recruitment pattern and increasing stability of the sacroiliac joint by using a pelvic belt may cause decreasing perception of difficulty during ASLR.
This research has some limitations. We did not measure the activation of transversus abdominis and pelvic floor muscles. In addition, we did not measure pelvic motion when recording the effect of muscle activity with a pelvic belt. Therefore, pelvic motion during ASLR using a pelvic belt remains unclear. The activity of the transversus abdominis, pelvic floor muscles, and pelvic motion during ASLR performance in the leg of the subjective heavier side should be evaluated in future investigations.
This study suggests that using a pelvic belt can decrease the perception of difficulty during ASLR and that the pelvic belt may improve impairment of load transfer between the trunk and pelvis.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.