AbstractIt is important that compensatory lateral movement of the pelvis does not occur during side-lying hip abduction (SHA). The purpose of the present study is to investigate the effects of abdominal hollowing and abdominal bracing during SHA on pelvic lateral rotation (PLR) and the electromyography activity of the gluteus medius, quadratus lumborum (QL), external oblique abdominis (EO) and internal oblique abdominis (IO). A total of 22 healthy male adults participated in the study. The subjects performed three conditions in side-lying in random order: SHA with abdominal hollowing (SHA-AH), SHA with abdominal bracing (SHA-AB), and SHA without any condition (SHA-WC). The angle of PLR in SHA-AB was significantly lower compared to SHA-AH and SHA-WC, and angle of PLR in SHA-AH was significantly lower than that in SHA-WC. The muscle activity of the QL was significantly greater for SHA-AB compared to SHA-AH and SHA-WC. The muscle activity of the EO was significantly greater for SHA-AB compared to SHA-AH and SHA-WC. And the muscle activity of the EO for SHA-AH was significantly greater than that for SHA-WC. The muscle activity of the IO was significantly greater for SHA-AH and SHA-AB compared to SHA-WC. Based on these results, we suggest that abdominal bracing increases the muscle activity of QL, EO, and IO, and decreases the angle of PLR compare to abdominal hollowing during SHA.
INTRODUCTIONThe gluteus medius (GM) plays an important role in hip abduction and the dynamic stabilization of the pelvis while walking (Al-Hayani, 2009). The hip abductor muscles enable single leg standing, which is primarily supported by the GM (Neumann, 2009). Given that weakness and dysfunction of the GM can cause back pain, hip joint pain, and iliotibial band friction syndrome, it is essential to rehabilitate and strengthen the GM (Fredericson et al., 2002; Nadler et al., 2002; Strauss et al., 2010).
Side-lying hip abduction (SHA) is recommended to effectively strengthen the GM (Distefano et al., 2009) and side-lying can facilitate the contraction of the hip abductor (Kendall et al., 2005). If compensatory movement occurs during SHA due to the action of the quadratus lumborum (QL), it can lead to the lateral flexion of the pelvis, resulting in lateral instability and impaired movement (Comerford and Mottram, 2001). Therefore, it is important that the pelvis does not rotate compensatively while reinforcing the GM (Sahrmann, 2002).
In a previous study, Cynn et al. (2006) used a pressure biofeedback unit to stabilize the trunk during SHA. The authors reported that the use of a pressure biofeedback unit was effective, as it reduced the pelvic lateral rotation (PLR) and increased the muscle activity of the GM while decreasing that of the QL. In another study, Park et al. (2010) demonstrated the effectiveness of performing SHA while wearing a pelvic compression belt to stabilize the pelvis because it increases the muscle activity of the GM and decreases that of the QL. Although the pelvic kinematic information was not investigated, the authors expected that their study results would reduce the compensatory lateral motion of the pelvis. Thus, in previous studies, a pressure biofeedback unit and a pelvic compression belt were used to increase the lumbo-pelvic stability during SHA.
Abdominal hollowing (AH) and abdominal bracing (AB) are commonly used to stabilize the trunk (Kahlaee et al., 2017). AH is a method of selectively contracting the transverse abdominis muscle and internal oblique abdominis (IO) by pulling the navel towards the vertebra (Hodges and Richardson, 1996). Furthermore, AH helps prevent excessive lordosis of the lower back and forward incline of the pelvis (Kisner and Colby, 2002). On the other hand, AB is a method of isometric cocontraction of all muscles in the trunk to fix the lumbar spine (McGill et al., 2003). AB increases the stability of the vertebrae against sudden perturbations and reduces the movement of the lumbar spine (Vera-Garcia et al., 2007).
Until now, studies using AH and AB to stabilize the trunk during SHA have been lacking. In addition, the effects of AH and AB on the angle of PLR during SHA have not been studied. For that reason, we investigated the effects of AH and AB during SHA on the angle of PLR and the electromyography (EMG) activity of the GM, QL, external oblique abdominis (EO) and IO. Since previous research has demonstrated that stabilizing the trunk during SHA reduces PLR (Cynn et al., 2006), in the present study, we hypothesized that AH or AB would also reduce PLR during SHA.
MATERIALS AND METHODSSubjectsThe study was conducted with 22 healthy male adults (Table 1). Candidates who were unable to perform hip abduction due to pain in the back, pelvis, or legs, those with orthopedic/neurosurgical diseases or malformation/functional disorders, as well as those who were unable to perform tasks due to a mental disorder or disability, were excluded from the study. The study was approved by the university’s Institutional Review Board (approval number: 1040621-201705-HR-008-02) and written consent was obtained from all participants before the study was launched.
Three-dimensional ultrasonic motion analysis systemA three-dimensional motion analysis system (CMS 70P, Zebris Medizintechnik GmbH, Isny im Allgäu, Germany) was used to measure the angle of PLR during SHA. It consists of a CMS 70P basic unit transmitting data, an MA-XX measuring unit with three ultrasonic transmitters, a cable adapter, ultrasound body triple markers, and a computer system. The sampling rate was set to 30 Hz and the data were analyzed with Windata 1.71 software. A triple marker was placed in the center of the pelvis with a strap fixed at the height of the posterior superior iliac spine on both sides of the pelvis (Oh et al., 2007).
Surface EMG recording and data processingSHA was performed in the dominant leg. The EMG activity of the GM, QL, EO and IO of the leg for which abduction was performed was collected using a TeleMyo DTS EMG (Noraxon Inc., Scottsdale, AZ, USA). A disposable single surface electrode with the Ag/Agcl material was used. To minimize skin resistance, the hair was removed with a shaver; furthermore, using by fine sandpaper, the skin was rubbed 2–3 times to remove the corneum. Fat on the skin surface was removed with an alcohol swab and electrodes were attached to each muscle. For the GM, the electrodes were attached to about one-third of the way to the body on the condyle between the iliac crest and the femur, and for the QL, the electrodes were attached to a modestly slanted area located approximately 4 cm to the left from the belly of the erector spinae muscle that meets with the iliac crest and the middle of the 12th rib (Cynn et al., 2006; Park et al., 2010) For the EO, the electrodes were located in inferior and lateral to the 8th rib, and for the IO, they were placed approximately 2 cm downwards toward the lower part of the trunk from the anterior superior iliac spine (Suehiro et al., 2014).
The EMG signal processing was analyzed with Myo-Research Master Edition 1.06 XP software. The sampling rate was set to 1,500 Hz and the amplified waveform was filtered using a 20- to 450-Hz bandpass filter and a notch filter to remove 60-Hz noise. All collected EMG signals were processed with the root mean square and the signals collected from each muscle were normalized with the % maximal voluntary isometric contraction (%MVIC). The MVIC measurement postures of the targeted muscles were measured using Kendall’s method (Kendall et al., 2005). The MVIC of each muscle was performed 3 times for 5 sec. The average value was obtained by calculating the average value for each of the 3 sec excluding the first and the last seconds.
Experimental proceduresBefore the experiment, the participants were provided with a full explanation of AH and AB, and each exercise was trained for five minutes to ensure that the participants could perform each exercise. SHA with AH (SHA-AH), SHA with AB (SHA-AB), and SHA without any condition (SHA-WC) were conducted in a random order. To prevent muscle fatigue and learning effects, the participants took a five-minute break between each condition (Sykes and Wong, 2003).
The subjects were asked to lie on a treatment table with a nondominant leg against the table while straightening the trunk, pelvis, and the dominant leg. For the nondominant leg on the table, the hip joint was bent at 45° and the knee joint was bent at 90° to provide stability and comfort for the trunk (Selkowitz et al., 2013). With a goniometer and a target bar, the subject’s hip joint abduction angle was set at 25°, as commonly applied in the GM’s muscle testing (Park et al., 2010).
To measure the angle of PLR, each condition (AH, AB, WC) was conducted, then hip joint abduction was performed at the point where the target bar was hit (Fig. 1A). A total of three trials were performed and the average value of the resulting three measurements was used for further data analysis. To measure the EMG amplitude, the subjects performed each condition (AH, AB, WC) and then conducted the hip joint abduction for five seconds so that the knee hit the target bar (Fig. 1B). The measurements were conducted three times. The EMG signals collected for 3 sec excluding the first and last seconds, as well as the average value for the EMG signals measured three times, were used for further data analysis. All measurements were performed keeping the torso, hip and leg straight.
Statistical analysesStatistical analyses were performed using the PASW Statistics ver. 18 (SPSS Inc., Chicago, IL, USA). One-way repeated-measures analysis of variance was used to compare the differences in the angle of PLR and EMG amplitude of GM, QL, EO, and IO among three conditions (SHA-AH, SHA-AB, and SHA-WC). Statistical significance was set at 0.05 and the post hoc Bonferroni test was used for multiple pairwise comparisons.
RESULTS
Fig. 2 shows the results of the angle of PLR under three conditions (SHA-AH, 5.36±2.77; SHA-AB, 4.23±1.81; SHA-WC, 6.52±2.54). Significant differences in the angle of PLR among the three conditions were observed (F[2, 42]=19.349, P<0.001). post hoc analysis indicated that the angle of PLR for SHA-AB was significantly lower than those of SHA-AH (P<0.001) and SHA-WC (P=0.003). Furthermore, the angle of PLR for SHA-AH was significantly lower than that for SHA-WC (P=0.019).
Table 2 shows the result of the EMG activity of each muscle under three conditions. The post hoc analysis results demonstrated that the muscle activity of the QL was significantly greater for SHA-AB compared to SHA-AH (P<0.001) and SHA-WC (P=0.031). The muscle activity of the EO was significantly greater for SHA-AB compared to SHA-AH (P<0.001) and SHA-WC (P<0.001). The muscle activity of the EO for SHA-AH was significantly greater than that for SHA-WC (P<0.001). The muscle activity of the IO was significantly greater for SHA-AH (P< 0.001) and SHA-AB (P<0.001) compared to SHA-WC.
DISCUSSIONThe purpose of the present study was to investigate the angle of PLR and the muscle activities of GM, QL, EO, and IO under three conditions.
In this study, the angle of PLR showed the significantly smallest amount of change with SHA-AB condition than with other conditions. Furthermore, SHA-AH showed significantly less movement than the SHA-WC condition and a significantly higher movement than the SHA-AB condition. Therefore, these results suggest that AB can reduce the PLR more than AH during SHA. This finding is consistent with the results of previous studies demonstrating that AB is more effective than AH to maintain the lumbo-pelvic stability (Grenier and McGill, 2007; Vera-Garcia et al., 2007). However, contrary to our results, the comparison of Suehiro et al. (2014) for AH and AB during hip extension performance in the prone position yielded no significant difference in terms of kinematics. This suggests that AH can improve the anteroposterior stability of the lumbo-pelvic region more than lateral stability by posteriorly tilting the pelvis and reducing the lordotic curve of the lumbar spine.
Furthermore, previous studies using a pressure biofeedback unit and a pelvic compression belt to stabilize the trunk during SHA showed a significant increase in the muscle activity of the GM and a significant decrease in the muscle activity of the QL (Cynn et al., 2006; Park et al., 2010) However, the GM showed no significant difference in the present study. Conversely, in SHA-AB which showed the lowest angle of PLR, the muscle activity of the QL was increased by 44.07% as compared to SHA-AH, and by 24.57% as compared to SHA-WC. These results suggest that AB causes isometric cocontraction for trunk muscles, thereby can cause isometric cocontraction of the QLs on both sides. When one side of the QL contracts, it causes the pelvis to rotate (Comerford and Mottram, 2001). However, if the QLs on both sides are isometric cocontraction, the lateral movement of pelvis is not expected to occur, and the results of our study (SHA-AB condition showed the lowest angle of PLR) support this. Thus far, studies have focused on reducing the QL muscle activity to avoid PLR during SHA (Cynn et al., 2006; Park et al., 2010). However, in our study, AB decreased PLR and increased the QL muscle activity during SHA. Furthermore, the medial part of the QL provides lumbo-pelvic stability through segmental attachment of the lumbar spine (Richardson et al., 1999). Therefore, we suggest that when performing SHA-AB, a decrease in the QL should not be claimed as the correct method to reduce PLR. Rather, a change of the PLR, which is kinematic data, should be considered.
In the present study, the muscle activity of the EO increased for SHA-AB by 28.99% more than SHA-AH, and by 134.7% more than SHA-WC. Also, it was significantly increased for SHA-AH more than SHA-WC by 81.95%. These results are consistent with the results of previous studies demonstrating that AB has a higher muscle activity than AH in the EO (Grenier and McGill, 2007; Vera-Garcia et al., 2007). The muscle activity of the IO for SHA-AH increased by 165.62% more than SHA-WC, and SHA-AB increased by 168.98% more than SHA-WC. Therefore, we suggest that AH and AB can contribute to the reduction of PLR using the abdominal oblique muscles to secure the stability of the trunk during SHA.
This study has several limitations. First, due to our focus on healthy male adults, it is difficult to generalize the results of the present study to other population groups. Second, we could not confirm whether the muscle activity on both sides of the QL and the abdominal oblique muscles on both sides increased when AB was conducted, because we only measured the muscle on the side of the hip joint that was abducted. In future studies, it is necessary to identify muscles of trunk on both sides. Third, due to the cross-sectional study design of the present research, we could not determine the long-term effects.
In conclusion, we suggest that both AB and AH can reduce PLR during SHA. And we suggest that AB increases the muscle activity of QL, EO, and IO, and reduces the PLR more than AH during SHA.
REFERENCESComerford MJ, Mottram SL. Movement and stability dysfunction--contemporary developments. Man Ther. 2001;6:15–26.
Cynn HS, Oh JS, Kwon OY, Yi CH. Effects of lumbar stabilization using a pressure biofeedback unit on muscle activity and lateral pelvic tilt during hip abduction in sidelying. Arch Phys Med Rehabil. 2006;87:1454–1458.
Distefano LJ, Blackburn JT, Marshall SW, Padua DA. Gluteal muscle activation during common therapeutic exercises. J Orthop Sports Phys Ther. 2009;39:532–540.
Fredericson M, White JJ, Macmahon JM, Andriacchi TP. Quantitative analysis of the relative effectiveness of 3 iliotibial band stretches. Arch Phys Med Rehabil. 2002;83:589–592.
Grenier SG, McGill SM. Quantification of lumbar stability by using 2 different abdominal activation strategies. Arch Phys Med Rehabil. 2007;88:54–62.
Hodges PW, Richardson CA. Inefficient muscular stabilization of the lumbar spine associated with low back pain. A motor control evaluation of transversus abdominis. Spine (Phila Pa 1976). 1996;21:2640–2650.
Kahlaee AH, Ghamkhar L, Arab AM. Effect of the abdominal hollowing and bracing maneuvers on activity pattern of the lumbopelvic muscles during prone hip extension in subjects with or without chronic low back pain: a preliminary study. J Manipulative Physiol Ther. 2017;40:106–117.
Kendall FP, McCreary EK, Provance PG, Rodgers M, Romani W. Muscles: testing and function with posture and pain. 5th ed. Baltimore: LWW; 2005.
Kisner C, Colby LA. Therapeutic exercise foundations and techniques. 4th ed. Philadelphia (PA): FA Davis; 2002.
McGill SM, Grenier S, Kavcic N, Cholewicki J. Coordination of muscle activity to assure stability of the lumbar spine. J Electromyogr Kinesiol. 2003;13:353–359.
Nadler SF, Malanga GA, Bartoli LA, Feinberg JH, Prybicien M, Deprince M. Hip muscle imbalance and low back pain in athletes: influence of core strengthening. Med Sci Sports Exerc. 2002;34:9–16.
Neumann DA. Kinesiology of the musculoskeletal system: foundations for rehabilitation. 2nd ed. St Louis (MO): Mosby; 2009.
Oh JS, Cynn HS, Won JH, Kwon OY, Yi CH. Effects of performing an abdominal drawing-in maneuver during prone hip extension exercises on hip and back extensor muscle activity and amount of anterior pelvic tilt. J Orthop Sports Phys Ther. 2007;37:320–324.
Park KM, Kim SY, Oh DW. Effects of the pelvic compression belt on gluteus medius, quadratus lumborum, and lumbar multifidus activities during side-lying hip abduction. J Electromyogr Kinesiol. 2010;20:1141–1145.
Richardson C, Jull G, Hodges P, Hides J. Therapeutic exercise for spinal segmental stabilization in low back pain. London: Churchill Livingstone; 1999.
Sahrmann SA. Diagnosis and treatment of movement impairment syndromes. St Louis (MO): Mosby; 2002.
Selkowitz DM, Beneck GJ, Powers CM. Which exercises target the gluteal muscles while minimizing activation of the tensor fascia lata? Electromyographic assessment using fine-wire electrodes. J Orthop Sports Phys Ther. 2013;43:54–64.
Strauss EJ, Nho SJ, Kelly BT. Greater trochanteric pain syndrome. Sports Med Arthrosc Rev. 2010;18:113–119.
Suehiro T, Mizutani M, Watanabe S, Ishida H, Kobara K, Osaka H. Comparison of spine motion and trunk muscle activity between abdominal hollowing and abdominal bracing maneuvers during prone hip extension. J Bodyw Mov Ther. 2014;18:482–488.
Fig. 1(A) Measurement of the angle of pelvic lateral rotation in side-lying hip abduction. (B) Measurement of muscles activity of the gluteus medius, quatratus lumborum, external oblique, and internal oblique. 
Fig. 2Comparison of the angle of pelvic lateral rotation between the conditions. SHA-AH, side-lying hip abduction with abdominal hollowing; SHA-AB, SHA with abdominal bracing; SHA-WC, SHA without any condition. Means and standard deviations are denoted by bars, respectively. *P<0.05. 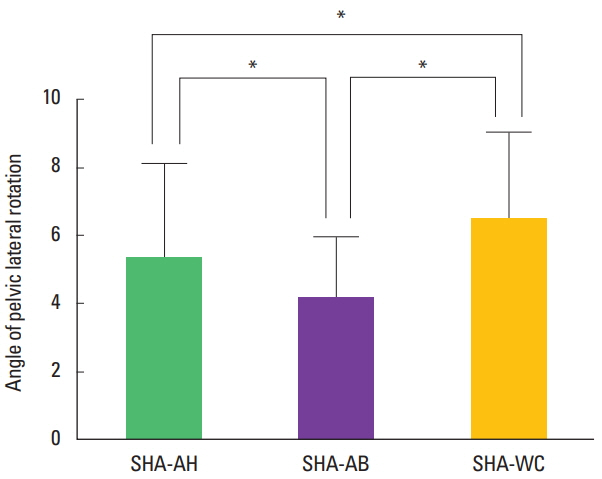
Table 1General characteristics of subject (n=22)
Table 2Electromyography activity of each muscle among three conditions
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||