INTRODUCTION
Inflammation plays a role in several diseases such as coronary artery disease, obesity-related insulin resistance, atherosclerosis, cancer, and Alzheimer disease (Lee et al., 2004; Shew et al., 1993; Willoughby et al., 1975; Zamora et al., 2000). Lipopolysaccharide (LPS) is an endotoxin from the outer membrane of Gram negative bacteria which activates pro-inflammatory cytokines (Wu et al., 2001). Nitric oxide (NO) is produced endogenously by a family of NO synthases (NOSs) with a wide range of physiological and pathophysiological actions (Moncada et al., 1991; Nathan and Xie, 1994). NOS enzymes are classified into two groups. One group, constitutive NO synthase is constitutively present in several cell types (e.g., neurons and endothelial cells) (Liu and Hotchkiss, 1995). The other group, inducible NO synthase (iNOS), which is expressed in various cell types, including macrophages. iNOS is induced in response to pro-inflammatory cytokines and bacterial LPS (Rockey et al., 1998). Excessive and prolonged iNOS-mediated NO generation has been linked with inflammation and tumorigenesis.
Cyclooxygenase-2 (COX-2) is an inducible enzyme catalyzing the conversion of arachidonic acid to prostaglandins. Recent studies have suggested that increased levels of prostaglandins and cyclooxygenase activity may play important roles in multiple epithelial cancers such as colon carcinoma (Dubois et al., 1998). COX-2-derived bioactive lipids, including prostaglandin E2 (PGE2), are potent inflammatory mediators that promote tumor growth and metastasis by stimulating cell proliferation, invasion, and angiogenesis (Mann et al., 2005). Therefore, high levels of prostaglandins may promote the development of malignancy (Yoshimura et al., 2005).
Phellinus igniarius (PI) is the dried fruiting body of PI named by parasitizing on the trunk of Morus alba L., Morus Moraceae, which was mainly distributed in China, Japan, Mongolia, Korea and some other Asian countries as well as America and Africa. It can also parasitize on other plants like Populus, Salix babylonica L., Betula, etc. As an excellent and precious medicinal fungus, PI has been widely used as health booster and ancient herbal medicine in East Asian countries, especially in Korea, China, and Japan. According to traditional applications, PI has various pharmacological activities including regulating blood glucose, improving blood circulation, hepato-protecting and enhancing immunologic function, etc. Also, PI has been experimentally demonstrated to possess antitumor, immuno-modulatory, anti-inflammatory, antioxidant, antihyperlipidemic and anti-diabetic activities (Chen et al., 2016).
The objective of this study was to investigate the effect of antioxidant and anti-inflammation of PI on LPS-induced RAW264.7 cells.
MATERIALS AND METHODS
Materials
PI was kindly donated by Dong-Woo Co. (Seoul, Korea). RAW-264.7 mouse macrophage cell lines were purchased from American Type Culture Collection. Sodium nitrite, Dimethylsulfoxide, 3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyl, 1,1-diphenyl-2-picrylhydrazyl, Ascorbic Acid, LPS, and Griess reagent were purchased from Sigma Chemical Co. (St. Louis, MO, USA). Serum free Dulbecco Modified Eagle Medium (DMEM) was purchased from GenDEPOT Co. (Houston, TX, USA). Phosphate buffered saline, fetal bovine serum, penicillin and streptomycin were purchased from GibcoBRL Co. (Grand Island, NY, USA).
Sample preparation
To obtain the water extract of PI, 200 g of PI was added to distilled water, and extraction was performed by heating at 100°C, concentrated with a rotary evaporator and lyophilized. The resulting powder, weighing 10 g, was dissolved in saline.
Cell culture
Mouse macrophage cell line, RAW264.7 was cultured in DMEM supplemented with 10% heat-inactivated FBS, 100-U/mL penicillin and 100-μg/mL streptomycin. The cells were maintained at 37°C in 5% CO2–95% O2 in a humidified cell incubator.
Cytotoxicity assay
Cell viability was determined using the 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay kit as per the manufacturer’s protocols. In order to determine the cytotoxicity of PI were treated with PI at concentration of 50, 100, 200, and 400 μg/mL. Cultures of the control group were left untreated. Ten microliter of the MTT labeling reagent was added to each well, and the plated were incubated for 4 hr. Solubilization solution of 100 μL was the added to absorbance was then measured with a microtiter plate reader (Bio-Tek, Winooski, VT, USA) at a test wavelength of 195 nm and a reference wavelength of 690 nm. Optical density (O.D.) was calculated as the difference between the absorbance at the reference wavelength and that at the test wavelength. Percent viability was calculated as (O.D. of drug-treated sample/control O.D.)×100.
Determination of NO production
In order to determine the effect of PI on NO production, the amount of nitrite in the supernatant was measured using a commercially available NO detection kit. After collection of 100 μL of supernatant, 50 μL of N1 buffer was added, and the plate was incubated at room temperature for 10 min. N2 buffer was then added, and the plate was incubated at room temperature for 10 min. the absorbance of the content of each well was measured at 450 nm. The nitrite concentration was calculated from a nitrite standard curve.
RNA isolation and realtime PCR
Total RNA was isolated from RAW264.7 cells by TRIzol (Thermo Scientific, Waltham, MA, USA) and converted to cDNA using High-Capacity cDNA reverse Transcription Kits (Thermo Scientific). Real-time PCR was performed with StepOnePlus Real-Time PCR System (Thermo Scientific). PCR reactions were performed in 20-μL reactions with SYBR Green Realtime PCR Master Mix (Toybo, Osaka, Japan). The following primers were used for real-time PCR (Table 1).
Measurement of PGE2
Assessment of PGE2 synthesis was performed using a commercially available PGE2 competitive enzyme immunoassay kit (Amersham Pharmacia Biotech Inc., Piscataway, NJ, USA). Cells were lysed and cell lysates and standard were put into different wells on the goat anti-mouse IgG-coated microtiter plate provided in the kit. Mouse anti-PGE2 antibody and peroxidase-conjugated PGE2 were added to each well, and the plate was incubated at room temperature and shaken for 1 hr. The wells were washed, and 3,3′,5,5′-tetramethylbenzidine/hydrogen peroxide solution was added. The plate was incubated at room temperature with shaking, and the reaction was stopped after 30 min through the addition of H2SO4. The absorbance of the content of each well was then measured at 450 nm.
Measurement of free radical scavenging activities by DPPH assay
The free radical scavenging capacity of PL was analyzed by using 2,2-diphenyl-1-picrylhydrazyl (DPPH). PL was diluted with 0.1 M acetic acid buffer (pH, 5.5) at various concentration (50, 100, 200, 400 μg/μL). Ascorbic acid was used as a positive control. A volume of 40 μL of samples and 60 μL of ethanol (with or without 0.1 mM DPPH) were mixed in 96-well plate at room temperature for 30 min, and the absorbance at 517 nm was measured. The DPPH scavenging effect was calculated as follows: Scavenging effect (%)=(1−sample O.D./control O.D.)×100.
RESULTS
Cell cytotoxicity
The viabilities of cells incubated with PI at 50, 100, 200, and 400 μg/mL for 24 hr were 96.31%±8.19%, 97.79%±4.69%, 96.14%±6.08%, and 91.38%±5.79% of the control value, respectively. The MTT assay revealed that PI exerted no significant cytotoxicity in the RAW264.7 macrophage cells (Fig. 1).
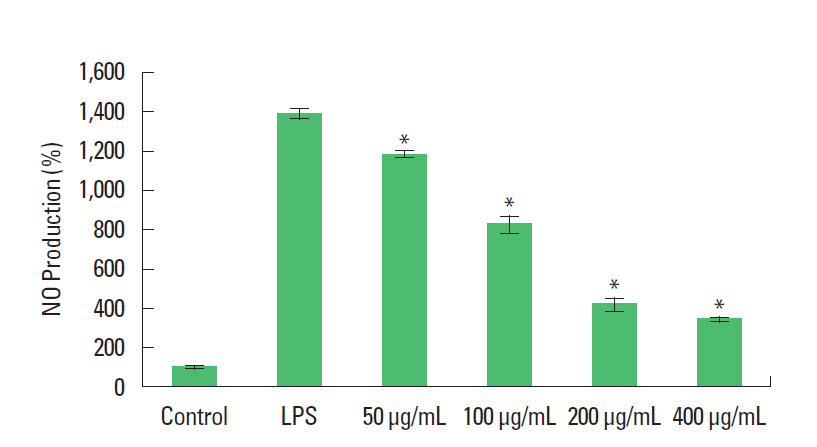
Effect of PI on NO synthesis
From NO detection assay, after 24 hr of exposure to LPS, the amount of nitrite was increased to 1,392%±27.52% of the control, while decreased to 1,187.44%±21.62%, 827.33%±41.40%, 417.36%±30.70%, and 342.23%±9.09% of the control by treatment with PI at 50, 100, 200, and 400 μg/mL (Fig. 2).
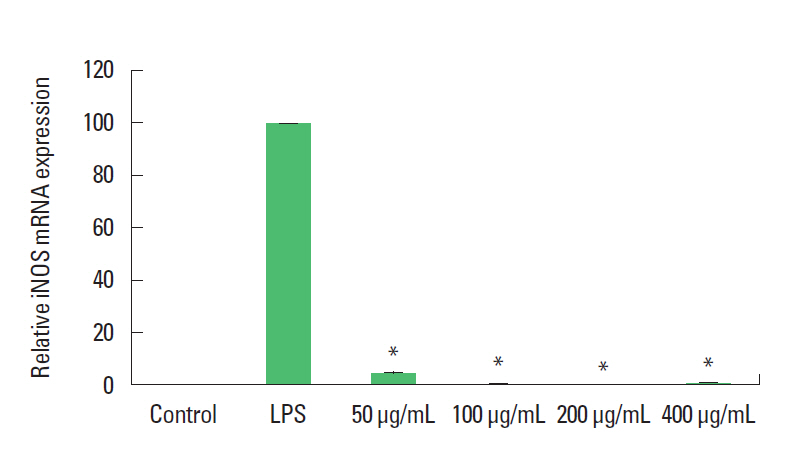
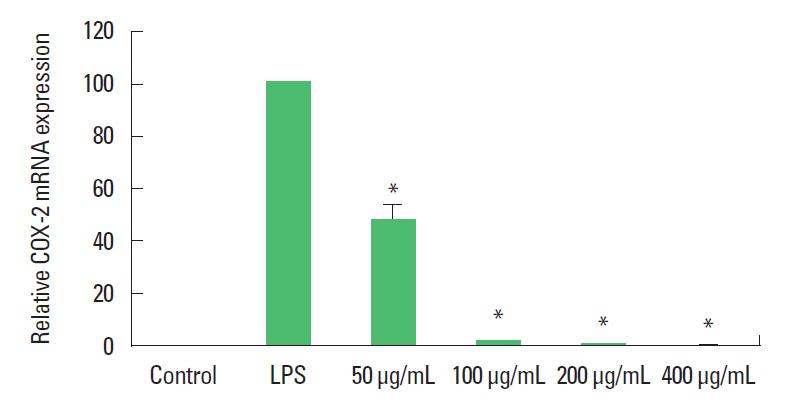
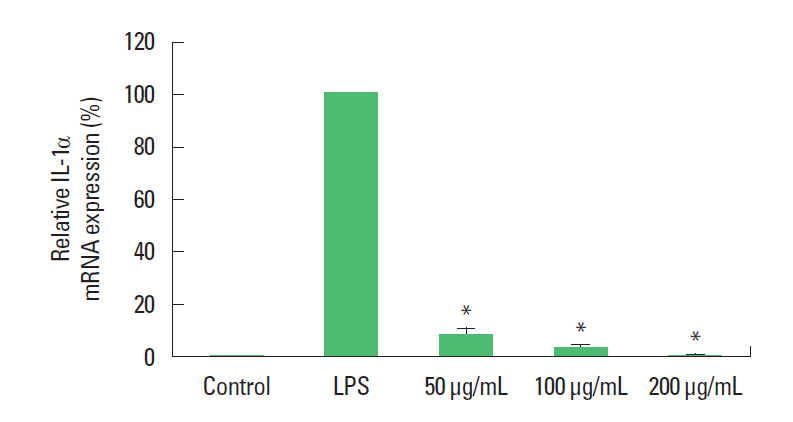
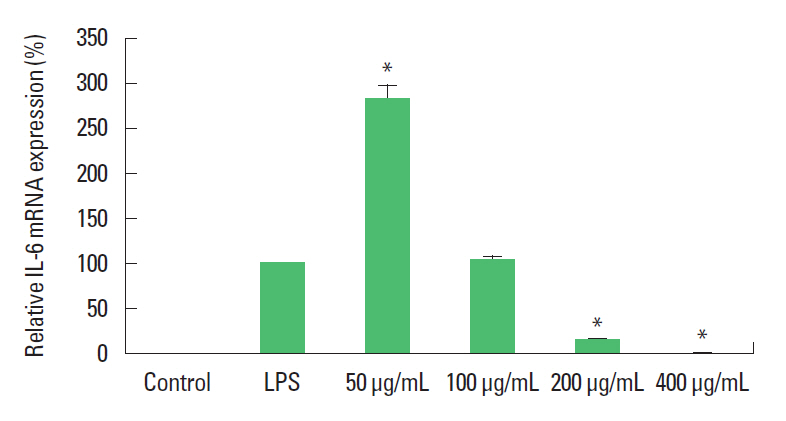
Effect of PI on mRNA expressions of cytokines
Real-time PCR analysis of the mRNA levels of COX-2, iNOS, IL-1α, IL-β, IL-6, and tumor necrosis factor (TNF)-α were performed in order to provide an estimate of the relative levels of expressions of these genes. In the present study, the mRNA expression levels of COX-2, iNOS, IL-1α, IL-β, IL-6, and TNF-α were increased in the LPS treated groups compared to the control groups. And, the mRNA expression levels of COX-2, iNOS, IL-1α, IL-β, IL-6, and TNF-α were decreased in the PI treated groups compared to the LPS treated groups (Figs. 3Fig. 4Fig. 5Fig. 6Fig. 7–8).
Effect of PI on PGE2 synthesis
From PGE2 immunoassay, after 24 hr of exposure to LPS, the amount of PGE2 was increased from 251.45±2.50 pg/well to 499.45±0.19 pg/well, while decreased to 441.81±1.73 pg/well, 423.22±5.91 pg/well, 331.59±0.38 pg/well, and 382.20±4.52 pg/well by the treatment with PI at 50, 100, 200, and 400 μg/mL (Fig. 9).
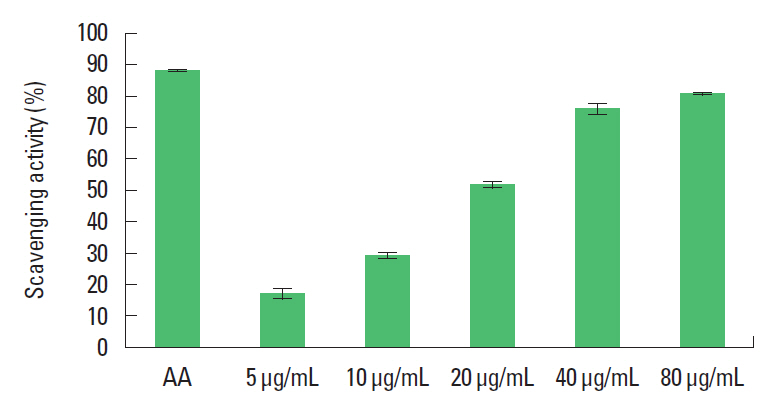
Effect of PI on free radical scavenging capacity by DPPH assay
From DPPH assay, the free radical scavenging capacities were increased to 17.29%±1.64%, 29.54%±0.84%, 51.87%±0.92%, 76.02%±1.54%, 80.86%±0.29% by the treatment with PI at 5, 10, 20, 40, and 80 μg/mL (Fig. 10).
DISCUSSION
The Characters of Drugs written by Quan Zhen in the early Tang Dynasty described the medical applications of PI, which was mainly used for hemorrhage, hemostasis and some diseases associated with female menstruation (Chen et al., 2016). In this study, we investigated the antioxidative and the anti-inflammatory effect of PI on RAW 264.7 macrophages cells.
Under normal physiological condition, NO is known to have an anti-inflammatory activity. However, NO has been reported to play an important role in the pathogenesis of inflammatory disorders under abnormal situation. Thus, the inhibition of NO production has been regarded as the potential therapeutic advance in the treatment of inflammatory diseases (Sharma et al., 2007). Like to NO, PGE2 has been established as a major component of anti-inflammatory response under normal physiological condition. However, PGE2 has been reported to be involved in tissue damage by inducing the production of matrix metalloproteinases in inflammatory disease (Blotman et al., 1982). Thus, PGE2 production inhibitors have been used for the treatment of human inflammatory diseases (McCoy et al., 2002).
Excessive NO production by iNOS causes pro-inflammatory effects (Bogdan et al., 2001). PGE2 as a principal mediator of inflammation is produced by COX-2. Cytokines as key modulators of inflammation have been view to participate in chronic inflammation (Smith et al., 2000). Among various cytokines, tumor necrosis factor-α (TNF-α), interleukin (IL)-1α (IL-1α), IL-1β, and IL-6 are included in key pro-inflammatory cytokines. These cytokines have been known to be involved in the pathology of inflammatory diseases. Thus, the down-regulation of these cytokines has been regarded as one of the important functions for the anti-inflammatory agents. In this study, we observed that PI effectively inhibits the expression of these cytokines.
In order to examine the effect of PI on RAW 264.7 cell cytotoxicity, we performed MTT assay. The viabilities of cells incubated with PI at 50, 100, 200, and 400 μg/mL were 96.31%±8.19%, 97.79%±4.69%, 96.14%±6.08%, and 91.38%±5.79% of the control value, respectively. Therefore, the MTT assay revealed that PI exerted no significant cytotoxicity in the RAW264.7 macrophage cells (Fig. 1).
NO is a type of ROS that has anti-inflammatory action, but it causes the destruction of host cells and tissue injury causes by induction of inflammatory reaction (Mann et al., 2005). From NO detection assay, after exposure to LPS, the amount of nitrite was increased to 1,392%±27.52% of the control, while decreased to 1,187.44%±21.62%, 827.33%±41.40%, 417.36%±30.70%, and 342.23%±9.09% of the control by treatment with PI at 50, 100, 200, and 400 μg/mL (Fig. 2). These results suggest that the inhibition of NO production by PI may reduce the tissue damage caused by the inflammatory reaction.
In addition, the production amount of NO was decreased, and the amount of mRNA expression at the transcription stage was confirmed. Realtime PCR analysis of the mRNA levels of COX-2, iNOS, IL-1α, IL-β, IL-6, and TNF-α were performed in order to provide an estimate of the relative levels of expressions of these genes. In the present study, the mRNA expression levels of COX-2, iNOS, IL-1α, IL-β, IL-6, and TNF-α were increased in the LPS treated groups compared to the control groups. And, the mRNA expression levels of COX-2, iNOS, IL-1α, IL-β, IL-6, and TNF-α were decreased in the PI treated groups compared to the LPS treated groups (Figs. 3Fig. 4Fig. 5Fig. 6Fig. 7–8).
And the amount of PGE2 that is the lowest level was confirmed. From PGE2 immunoassay, after exposure to LPS, the amount of PGE2 was increased from 251.45±2.50 to 499.45±0.19 pg/well, while decreased to 441.81±1.73, 423.22±5.91, 331.59±0.38, and 382.20±4.52 pg/well by the treatment with PI at 50, 100, 200, and 400 μg/mL (Fig. 9). It is supposed that PGE2 decreased by the decreased of NO and COX-2.
In order to measure the free radical scavenging ability, DPPH assay was used to measure the antioxidative effect of PI at 5, 10, 20, 40, and 80-μg/mL concentrations. The free radical scavenging capacities were increased to 17.29%±1.64%, 29.54%±0.84%, 51.87%±0.92%, 76.02%±1.54%, 80.86%±0.29% by the treatment with PI at 5, 10, 20, 40, and 80 μg/mL (Fig. 10). These results suggest that PI reduces the production of peroxidation by inhibiting active oxygenase.
These results suggest that PI can exert its anti-inflammatory and antioxidative effects probably by suppressing pro-inflammatory cytokines, resulting in the inhibition of PGE2 and NO synthesis.