Effects of communal exercise with visual and auditory feedback provided by a smart application on gait ability and fear of falling in Parkinson’s disease patients
Article information
Abstract
Parkinson’s disease is a chronically developing neurodegenerative disease showing typical motor symptoms of the following triad: resting tremor, freezing of gait, and bradykinesia-hypokinesia. In the present study, we investigated the effects of a communal exercise program, using the visual and auditory feedback provided by a smart application, to assess gait ability, fear of falling, and fall efficacy in Parkinson’s disease patients. Subjects consisted of 29 Parkinson’s disease patients who were non-demented individuals. The subjects were randomly divided into three groups: the control group (n= 9, CG), the communal exercise group using the smart application (n= 10, CCEG), and the individual exercise group using the smart application (n= 10, ICEG). The communal exercise program consisted of a warm up (10 min) followed by communal exercise using the smart application (40 min), and a cool down (10 min) for 3 days per week over 10 weeks. The results presented here show that velocity and cadence were significantly increased among groups. Step and stride length were significantly increased among times. Fear of falling and fall efficacy were significantly different among groups and times. In particular, fear of falling was lower and fall efficacy was higher in the CCEG than in the ICEG and CG. These findings indicate that 10 weeks of the communal exercise program using the smart application can be effective in improving gait ability, fear of falling, and fall efficacy in Parkinson’s disease patients.
INTRODUCTION
A slow, freezing gait is typical in people with Parkinson’s disease (PD) (Hausdorff, 2009). The risk of falling, loss of independence, and risk of mortality are increased as a result of gait related problems (Robinson et al., 2005). The experience of falling can increase a PD patient’s fear of falling, which may lead to further incidences of falling (Morris et al., 2010). The fear of falling limits their activity level, social activities, functional fitness, and independence (Lamout et al., 2012).
Regular exercise has been shown to improve physical and psychological activities for PD patients (Allen et al., 2010; Morris et al., 2010). However, it remains unclear how long these effects last and how these effects are sustained (Tomlison et al., 2012).
PD is a disease of the elderly, and it presents with complex symptoms such as disorders of cognition and language, depression, fatigue, self-care, communication, as well as motor disorders (Allen et al., 2010). Thus, it is necessary that exercise programs of PD patients consider various aspects to enhance flexibility, strength, endurance, coordination, and gait ability (de Paula et al., 2006). Furthermore, it is better to form an exercise group for social communication (Reuter and Engelhardt, 2002) and to use external stimuli like recently advanced visual and auditory feedback technology. According to previous studies, the benefits of external visual and auditory feedback are mediated by neural pathways to help internally guided movements in patients with PD (Elsinger et al., 2006; Georgy et al., 2012).
In the present study, we investigated the effects of a regular communal exercise program with a smart application, which has never been used for this kind of study to be able to overcome space/time as a visual and auditory feedback system on gait ability, fear of falling, and fall efficacy.
MATERIALS AND METHODS
Subjects
Subjects consisted of 29 PD patients who were non-demented and community-dwelling individuals. The subjects were randomly divided into three groups: Control group (n=9, CG), communal exercise group with smart application (n=10, CCEG) and individual communal exercise group with smart application (n=10, ICEG). Selection criteria was based on a diagnosis of idiopathic PD according to the department of neurosurgery of Y hospital, classification of modified Hoehn and Yahr (1967) stage 1 through 3, and an ability of gait independence. Subjects were excluded if they had other neurological problems such as, acute medical problems that could affect gait, a score below 23 on the Mini-Mental State Examination, or had fallen more than once in the previous year. The physical characteristics of the subjects are shown in Table 1.
Study design
Subjects were randomly separated into CG, CCEG and ICEG in order to evaluate gait ability, fear of falling, and fall efficacy before and after the 10-week communal exercise program.
Measures of gait
The GAITRite system (GAITRite, CIR systems Inc., Clifton, NJ, USA, 2008) is made of 5 m length walkway and 16,128 sensors. Over the walking of the subject, the system automatically detect pressures through the sensors, and delivers the data to the computer to calculate gait parameters. The subjects walk three times and the calculated average of the three trials was used to analyze the data.
Measures of fear of falling and fall efficacy
A “Fear Of Falling Questionnaire” (FOFQ, Tideiksaar, 1997), which consists of 11 questions with 4 scales, was used here (Cron-bach’s α=0.09). The “Korean Falls Efficacy Scale” (K-FES, Tinetti et al,, 1990) which consisted of 10 questions was also used here (Cronbach’s α=0.96). The questions focused on the fear of falling during a PD patient’s daily living activities, as follows: walking outdoors and indoors, using the toilet, taking a bath, taking a seat, standing and reaching up to a cabinet, or going up and down stairs.
Exercise intervention
Subjects performed a communal exercise program using a smart application for 60 min, three times per week, for a period of 10 weeks, which focused on improving their deep breathing, relaxation levels, flexibility, strength, balance, and gait pattern. The subjects and caregivers were instructed how to use the smart application and how to perform the exercise program. The exercise program used a smart application named “Parkinson home exercise application”, which has been developed by the Association of Physiotherapists in Parkinson’s Disease Europe (APPDE, 2009).
Data analysis
The data was analyzed by two-way repeated measures ANOVA and a Scheffe post-hoc test was performed. Statistical significance was set at P<0.05.
RESULTS
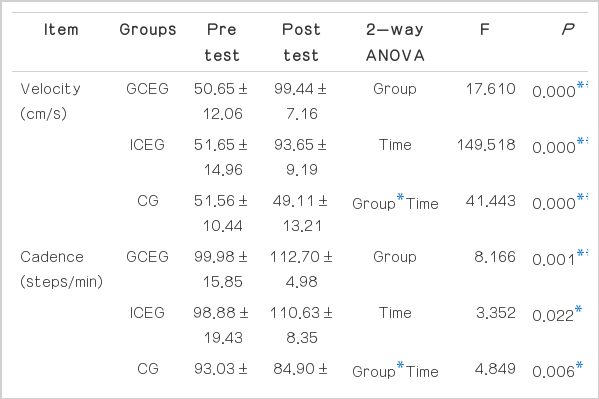
Changes to temporal gait ability after the 10 week communal exercise program using the smart application
The results are presented in Table 2. Velocity and cadence showed significant differences among group, time and interaction (P=0.000). After 10 weeks, velocity and cadence were higher in the CCEG and ICEG compared with the CG.
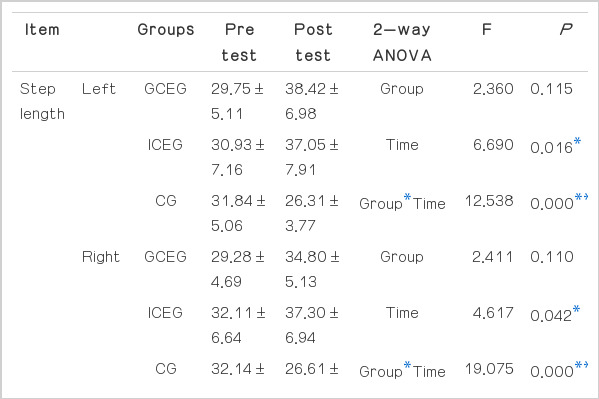
Changes in spatial gait ability after the 10 week communal exercise program using the smart application
The results are presented in Table 3. Step length and stride length showed no significant differences among the groups. However step length and stride length showed significant differences among time and interaction (Left: P=0.016, P=0.000, Right P= 0.042, P=0.000, Left: P=0.048, P=0.000, Right P=0.045, P= 0.000, respectively).
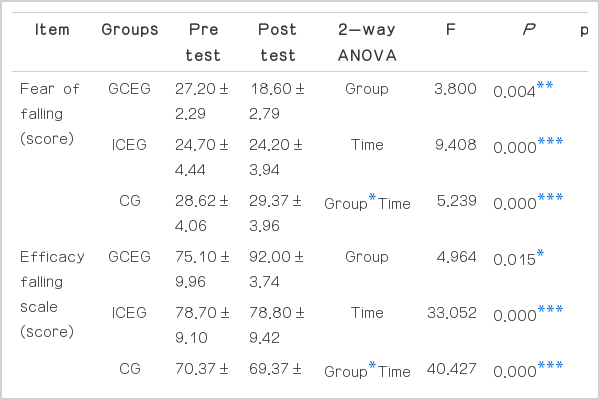
Changes in fear of falling and fall efficacy after the 10-week communal exercise program using the smart application
The results are presented in Table 4. Fear of falling and fall efficacy showed significant differences among group, time, and interaction (P=0.004, P=0.000, P=0.000, P=0.015, P=0.000, P= 0.000). After 10 weeks, fear of falling was higher in the CCEG compared with the ICEG and the CG and also in the ICEG compared with the CG. Fall efficacy was higher in the CCEG than the CG.
DISCUSSION
The present study investigates the effects of a 10-week communal exercise program, using a smart application for visual and auditory feedback in patients with PD, in regards to gait ability, fear of falling, and fall efficacy. A limitation of the current study is that no other studies have used a communal exercise program with a smart application to compare between communal exercise and individual exercise, so it is difficult to compare our findings to those in other studies.
Gait is one of the most essential daily living activities (McDermott et al. 2010). The gait velocity and cadence are chosen as important parameters to evaluate motor function and furthermore the quality of life after disease (Jonsdottir et al., 2009). External visual and auditory signs improved the spatiotemporal parameters of gait in PD patients (Kwakkel et al., 2007). In addition, communal exercise enhanced familiarity and improved social integrity functions (Reuter and Engelhardt, 2002). Emotional reactions, social interactions, and physical ability were significantly increased as a consequence of the group exercise undertaken by the PD patients (de Paula et al., 2006). The present study showed that cadence and velocity were significantly increased in the CCEG and the ICEG compared with the CG. However, step length and stride length showed no significant differences among groups, but were significantly increased as a function of time. Fear of falling and fall efficacy were significantly increased in the CCEG compared with the ICEG and the CG. Therefore, these findings indicate that the communal exercise program, with visual and auditory feedback of the smart application, was beneficial for gait ability, fear of falling, and fall efficacy. In addition, communal exercise enhances social communication.
In conclusion, a communal exercise program with visual and auditory feedback, using a smart application for PD patients, has a positive impact on both emotional and physical activities.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This work was supported by the National Research Foundation of Korea Grant funded by the Korean Government (NRF 2013 S1A5B5A07047602).