Modified laparoscopic intravesical nonrefluxing ureteral reimplantation with psoas hitch using a submucosal tunneling
Article information
Abstract
We aimed to study the safety and efficacy of the cystoscopy-assisted nonrefluxing ureteral reimplantation technique using submucosal tunneling during laparoscopic ureteroneocystostomy (UNC) with a psoas hitch in patients with distal ureter stricture after gynecologic surgery. We reviewed six female patients who underwent gynecological surgeries. All patients showed persistent postoperative distal ureter stricture or obstruction. These patients underwent laparoscopic nonrefluxing UNC with a psoas hitch using a submucosal tunneling technique combined with cystoscopy at our institute. They had corrective surgery at an average of 13.3 weeks after ureteral injury. The short-term success was confirmed either by voiding cystourethrography (VCU) or by diuretic isotope renal scan (MAG-3) conducted 3 months after the operation. None of the patients showed evidence of postoperative stricture at the reimplanted site and reflux on either MAG-3 renal scan or VCU. None of the patients showed major or minor complications during follow-up. It is safe and feasible to perform the laparoscopic nonrefluxing UNC with a psoas hitch using a submucosal tunneling technique combined with cystoscopy for ureteral stricture.
INTRODUCTION
In patients who undergo pelvic surgery including gynecologic procedures, ureteral injury is a sometimes recognized problem. It was reported that the incidence of complications during various pelvic and gynecologic procedures was 10.4% (Saidi et al., 1996), and the incidence of ureter injury was 4.3% (Ostrzenski et al., 2003).
Conventionally, open surgery has been the mainstay to treat ureteral injury. However, the trend of treatment is shifting toward predominantly laparoscopic-driven ureteral injury repair. The Laparoscopic urologic applications possess numerous advantages such as minimal postoperative pain, decreased hospitalization, a shorter convalescence, and better cosmesis (Modi et al., 2005).
Still, owing to its complexity and dexterity of anti-refluxing laparoscopic methods, most laparoscopic UNC are still performed with a refluxing ureteral reimplantation. Otherwise, when considering a nonrefluxing method, the operation is merely done extravesically.
Nevertheless, in 2006, we reported two cases of laparoscopic non-refluxing ureteral reimplantation with a psoas hitch using a submucosal tunneling technique combined with cystoscopy. Since then, we have utilized the technique to treat six more patients who recently had ureteral stricture due to distal ureter injuries during gynecologic surgery (Chung et al., 2006).
This study is to demonstrate the safety and the efficacy of laparoscopic non-refluxing ureteral reimplantation with a psoas hitch using a submucosal tunneling technique combined with cystoscopy, evaluating the results of the six patients.
MATERIALS AND METHODS
We reviewed the medical records of six female patients who underwent surgical repair in patients with distal ureter stricture after gynecologic surgery, from August 2004 to June 2013 at Gachon University Gil Medical Center. The surgical technique used for repair was laparoscopic nonrefluxing ureteral reimplantation with a psoas hitch using a submucosal tunneling technique combined with cystoscopy. We performed retrograde urethrography (RGP) for evaluation of the location and extent of ureteral stricture in the patients.
All operations were performed by a single surgeon. The surgical techniques were similar as previously reported (Chung et al., 2006). Under general anesthesia, the patient was placed in the lithotomy and Trendelenburg head-down position. Four ports were placed as following; an initial 10-mm camera port, two 12-mm ports lateral to the rectus muscle between the umbilicus and anterior superior iliac spine, and a 5-mm midline suprapubic port. After reflecting the colon, we identified the ureter, and umbilical tape was placed around the ureter to assist in ureteral exposure. The ureter was transected after ligation of the proximal end stricture. A traction suture was inserted into the proximal end of the ureter. After 200 mL of sterile water was instilled into the bladder, the space of Retzius was identified, and the bladder was mobilized by freeing its peritoneal attachments, reaching the psoas major muscle. After the bladder was incised transversely, the lower part of incised bladder was pexed to the tendon of the psoas major muscle over the iliac vessels with traction. A new hiatus in a fixed portion of the bladder was made with endoscopic scissors. The cystoscope was then inserted through the newly created hiatus into the intra-abdominal cavity. We used 7 Fr. cystoscopic forceps to grasp the traction suture in the ureter and to pull the ureter through the hiatus into the bladder.
The location of a new ureteral orifice was selected laparoscopically with the expectation of a tension-free anastomosis. Then we inserted a 22 Fr. cystoscope (Fig. 1A), and injected 2–3 mL of normal saline into submucosal layer of prearranged submucosal tunnel from the neoureteral opening to the new bladder hiatus with a 7 Fr. metal cystoscopic injection needle in order to make artificial bleb to facilitate submucosal tunneling (Fig. 1B). For creation of the submucosal tunnel, the artificial was incised and dissected by cystoscopic scissors under simultaneous inspection using both the laparoscope and cystoscope. After that, 7 Fr. cystoscopic forceps were inserted and crossed the submucosal tunnel, grasped the traction suture of the ureter, and pulled the ureter out of the new ureteral orifice (Fig. 1C). The length of submucosal tunnel was about 3 cm and 2.5 cm. An anastomosis between the ureteral end and the neoureteral opening was performed with four interrupted mucosa-to-mucosa sutures and two full-layer sutures (Fig. 1D). Then we inserted a 6 Fr. 24-cm double-pigtail (D-J) stent. After confirming the ureteral reimplantation was tension-free, the bladder was closed with continuous suture. A urethral Foley catheter was inserted, and a 10-mm flat Jackson-Pratt drain was placed in the intraperitoneal dependent portion.
Technique for forming new submucosal tunnel by combining cystoscopy with laparoscopy. (A) Cystoscope inserted into bladder for submucosal tunneling after cystostomy and psoas hitch. (B) Submucosal injection of normal saline at site selected site for submucosal tunnel. (C) Laparoscopic suturing after creation of new submucosal tunnel. (D) Neoureteral orifice after submucosal tunneling.
Approximately 2 weeks postoperatively, a cystography was performed, and when no leakage was observed, the urethral Foley catheter was then removed 14 days postoperatively. The D-J stent was removed with cystoscope postoperatively. One week after D-J stent removal, an IVP was performed, and a MAG-3 renal scan or VCU were performed.
RESULTS
The six patients treated with cystoscopy-assisted nonrefluxing ureteral reimplantation using submucosal tunneling during laparoscopic UNC with a psoas hitch were examined, and their demographic information is illustrated in Table 1. The mean age of the patients was 49.2 yr (41–76). The mean body mass index was 21.9 kg/m2 (20.1–23.4). Among the patients who underwent gynecologic surgery, one patient was diagnosed with cervical cancer (16.7%), two of them with post dilatation and curettage hemorrhage (16.7%) and four patients with myoma (66.7%). The patients had gynecologic procedure that included laparoscopic assisted vaginal hysterectomy (one patient, 16.7%), total laparoscopic radical hysterectomy (one patient, 16.7%), total laparoscopic hysterectomy (three patients, 50%) and total abdominal hysterectomy (one patient, 16.7%). The patients underwent the corrective surgery at an average of 13.3 weeks (1–19) after injury. Among these patients, three of them (50%) had left ureter injury, and the rest (50%) had right ureter injury. Prior to the surgical repair, all patients were treated with RGP, and three patients (50%) with ureteral stent insertion, two of them (33.3%) with percutaneous nephrostomy (PCN) insertion, and one patient (16.7%) received both PCN and ureteral stent insertion.
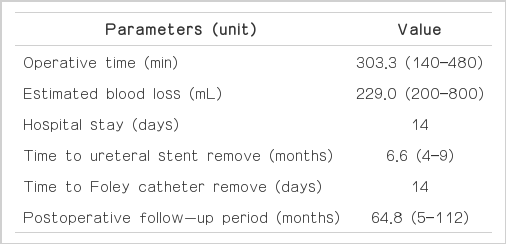
The intraoperative parameters were analyzed (Table 2). The mean operative time was 303.3 min (140–480), and average estimated blood loss was 391.7 mL (200–800). One patient was transfused with 2 pack red blood cells. The hospital stay duration for all patients was 14 days. The ureteral stents were removed cystoscopically 6.6 weeks (4–9) after insertion. Open conversion was not required in any of the cases. Postoperative results were also analyzed (Table 2). None of the patients showed evidence of stricture or reflux on IVP, MAG-3 renal scan and VCU. The mean follow-up period was 64.8 months (5-112). None of the others had major or minor complications during follow-up.
DISCUSSION
The incidence of ureter injuries during gynecologic surgery is reported to be approximately 0.1 to 2.5% (Koukouras et al., 2010; Park et al., 2012). Ureter injury may be caused by sutures, clips, staple ligation, crush injury, or thermal spread of electrocautery (Pompeo et al., 2013). If not detected intraoperatively, such injuries can cause numerous complications including decrease in renal function, fistulas, and sepsis (Sakellariou et al., 2002). When distal ureteral injury occurs, endourological procedures are initially considered. However, the outcome is generally not satisfactory, and the gold standard of repair is regarded to be open surgery (Narang et al., 2007). And, if the ureteral length is insufficient for reimplantation to the bladder, a psoas hitch is required, in order to ensure ureterovesical continuity (Juarez-Soto et al., 2014).
Laparoscopic surgery is usually more time-consuming than open surgery, and requires more surgical skill and experience. Complete reproduction of the open techniques is very challenging. Despite of such obstacles, laparoscopic surgery has the advantage of less pain, early ambulation, and rapid recovery, and is increasingly being performed in lower abdomen and pelvic surgery (Stolzenburg et al., 2006). It was reported that the first laparoscopic UNC was performed for vesicoureteral reflux (VUR) (Ehrlich et al., 1994). Such initial surgical techniques could not completely duplicate open techniques due to lack of intracorporeal suture skill. However, due to improvement of laparoscopic instruments and suturing techniques, reproduction of freehand intracorporeal suture, as performed in open UNC, became feasible (Kamat and Khandelwal, 2005).
There was outcome analysis of laparoscopic UNC with open UNC (Rassweiler et al., 2007). According to this study, it did not show significant difference between laparoscopic and open surgery groups in terms of post operative complications. Furthermore, the postoperative pain and hospital stay were shorter in laparoscopic surgery groups, showing better recover (Modi et al., 2005).
In UNC, it is of paramount importance to make an anti-reflux anastomosis without immediate or delayed obstruction. It was reported that VUR should be prevented in all reimplantation surgeries (Sakellariou et al., 2002) and advised construction of a submucosal anti-reflux channel in the bladder wall, through which diversion of the ureter is possible (Utrie, 1998). It is well known that congenital VUR is caused by the shortness of the submucosal tunnel of the ureter to the medial side of the bladder. Therefore, when performing open UNC, a new submucosal tunnel should be made in order to prevent VUR during ureteral reimplantation. However, the bladder mucosa is much too friable to manage with laparoscopic techniques, and submucosal tunneling technique is often difficult to perform without tearing it. During submucosal tunnel formation, forming a tunnel without ripping the bladder mucosa is especially challenging due to the limitation of laparoscopic instrument motion and angulation. The Lich-Gregoir extravesical approach, which uses multiple interrupted absorbable sutures when forming ureteral-mucosal anastomosis (Veale et al., 2007) is therefore used to overcome such difficulties (Azioni et al., 2010; Baldwin et al., 2005; McDougall et al., 1995). The advantages of such a technique are well-known for repair of VUR in children (Heidenreich et al., 2004), and when performing renal transplantation (Veale et al., 2007). However, the technical challenges are well-known, and therefore, it should be performed only in specialist centers and be performed by skilled surgeons (Azioni et al., 2010). Therefore complete replication of effective open surgery seemed still hard to be achievable.
With the aid of the self-developed technique which cystoscopically injects normal saline into the bladder forming a submucosal tunnel, we reported two successful cases of patients who experienced gynecologic iatrogenic distal ureter injury in 2006. The novel procedure enables laparoscopic submucosal tunnel completion without tearing bladder mucosa (Chung et al., 2006). Our laparoscopic procedure replicated the same steps used in open surgery.
With its extension, we performed six more cases and examined the safety and efficacy of the novel technique in patients who experience gynecologic iatrogenic distal ureter injury. None of the patients showed evidence of stricture or reflux on either IVP or MAG-3 renal scan and VCU after corrective surgery. During follow-up after corrective surgery, there was no complication at the anastomosis site, and more importantly, stricture and reflux were not observed including other major or minor complications. Based upon this study we are able to support the feasibility of concomitant intravesical nonrefluxing ureteral reimplantation with a psoas hitch using a submucosal tunneling technique
This study has some limitations. First, it was retrospectively performed, and therefore, analysis of parameters such as anatomic disruption due to underlying disease or previous surgery was not performed. Second, the sample size was relatively small. Due to the limited number of patients, further prospective studies with more controlled and detailed analysis of factors which might affect the outcome could be recommended. In addition, future studies may more strongly support the safety and efficacy of our technique.
Our novel technique of cystoscopy-assisted intravesical submucosal tunneling, along with a psoas hitch during laparoscopy, clearly not only duplicated the surgical principles of the open procedure but also produced the same results with no postoperative vesicoureteral reflux.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.