The effect of group training on pregnancy-induced lumbopelvic pain: systematic review and meta-analysis of randomized control trials
Article information
Abstract
Since there is lack of up to date consensus exists as to whether group training is effective in improving lumbopelvic pain (LPP) after pregnancy, a review of the recent evidences is needed. To determine the effect of group exercise training for the management of LPP among pregnant women compared with usual antenatal care. An electronic database search for relevant randomized control trials published in English from 2006 to 2015 was conducted. Articles with outcome measures of self-reported LPP, visual analogue scale and sick leave due to LPP after pregnancy were included. Quality of the included articles was rated using Physiotherapy Evidence Database (PEDro) scale and the pooled effect of self-reported LPP was obtained by Review Manager (RevMan 5) software. Significant effect of group training was detected over usual antenatal care or no treatment with P=0.0035 (95% confidence interval, −0.2348 to −0.0044). The results of this systematic review proposed that group training reduces LPP significantly better than routine antenatal care for pregnant women suffered from LPP.
INTRODUCTION
Low back pain (LBP) becomes the most common disabling condition throughout the world (Buchbinder et al., 2013; Hoy et al., 2014). LBP can affect the quality of life of peoples by preventing them from daily activities and making them dependent on their families (Hill et al., 2011). It is the leading cause of sick leave which affects the productivities of people to help the growth of their population and their family (Balagué et al., 2012).
LBP is also the major cause of depression and anxiety through different regions of the world and is a burden for the whole family to cover medical costs (Gore et al., 2012). LBP and pelvic among pregnant women is may be severe enough to cause significant pain and impaired physical functioning and the mean prevalence of LBP during pregnancy is more than 50% (Ansari et al., 2010; Mousavi et al., 2011). About 80% of pregnant women with back pain experience discomfort during daily activities and have difficulties with housework, activities in child-growing and job performance (Mens et al., 1996).
Huge number pregnant women consider that lumbopelvic pain (LPP) is a normal physiologic phenomenon of pregnancy and expected to spontaneously disappear after delivery. But For some women, it may be the beginning of lifelong chronic back pain as a result they may live with considerable impairment and disability (Davies et al., 2003).
In such way LPP among pregnant women is ignored and the present systematic review was designed to assess whether group exercise training is effective to manage LPP among pregnant women based on evidences.
MATERIALS AND METHODS
Objective
To determine the effect of group exercise training for the management of LPP among pregnant women compared with usual antenatal care.
Search strategy and inclusion
An electronic database search for relevant randomized control trials (RCTs) published in English (as translation funding was not available) was conducted from 2006 to 2015 on the following databases: PubMed through Hinari, Cochrane, Google scholar, CINAHL (Cumulative Index to Nursing and Allied Health Literature), MEDLINE, AMED (Allied and Complementary Medicine), Embase, and Physiotherapy Evidence Database (PEDro). Search key words included; randomized, controlled trials, pregnancy, LBP, LPP, group exercise and group training. Full texts of peer-reviewed relevant articles were retrieved, assessed and their reference lists were hand searched to identify further relevant studies.
Selection of studies
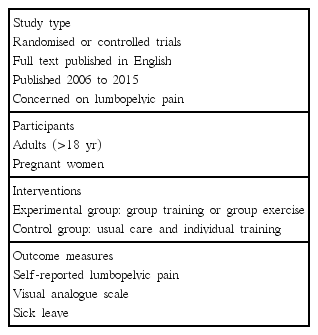
The method segment of listed trials was extracted and employed the predetermined inclusion criteria to screen for relevant full text trials. An article was removed from the list if it was determined not to meet the inclusion criteria. Studies were included for data extraction and analyses, if they met the predetermined inclusion criteria (Table 1).
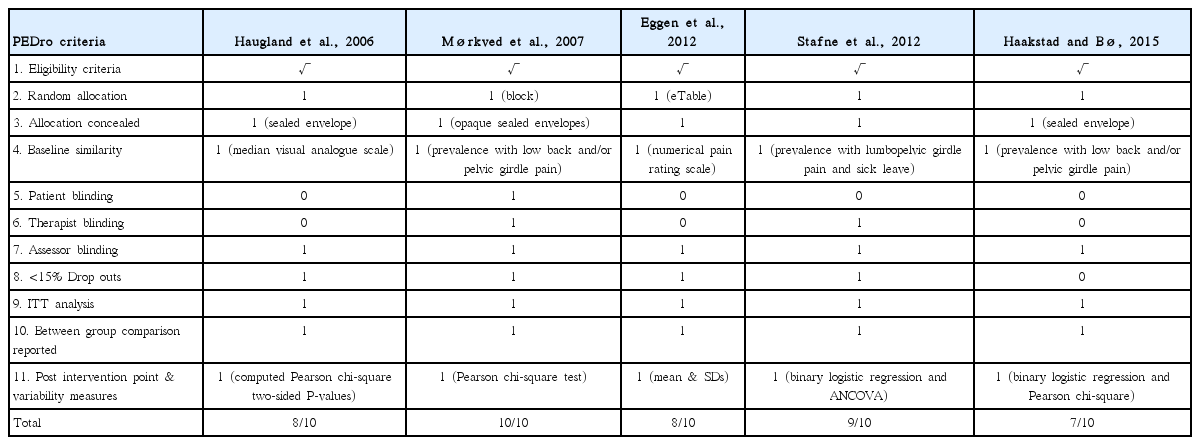
Quality assessment
For all the selected articles randomization method, blinding, selection criteria, and dropouts from follow-up were seen critically to assess risk of bias. Articles selected were critically appraised with 11 items PEDro scale scores extracted from the Physiotherapy Evidence Database (www.pedro.org.au). PEDro scale is a useful tool to assess the methodological quality of physical therapy and rehabilitation trials. Studies were excluded in subsequent analysis if the cutoff of 6 points was not reached on PEDro scale score (Table 2).
Data extraction and management
After searching relevant articles to this systematic review data were extracted from the studies using standard checklist. The information collected from each articles were as follows:
Patients details (including age, time since pregnancy, and LPP)
Method (the inclusion and exclusion criteria)
Intervention including (duration, intensity, and frequency)
The comparison intervention
Description of the group training approach
Outcome measures used and
Follow-up period
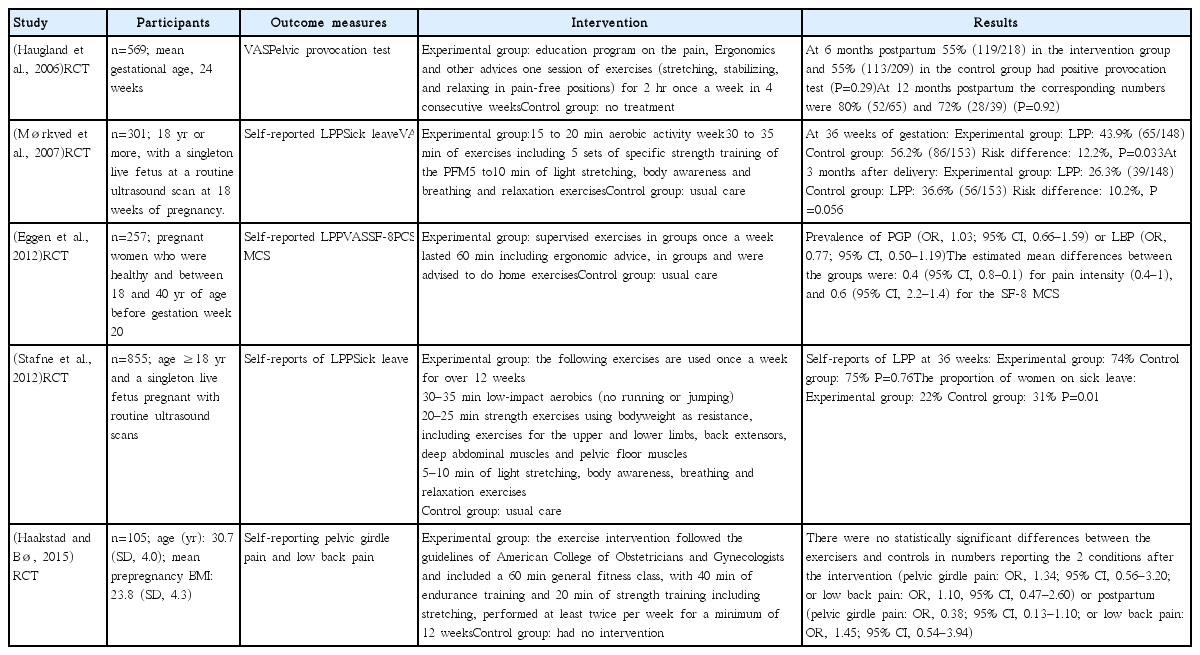
Data at baseline, post treatment and follow-ups were extracted for interested outcomes. Findings were putted in logical order, discussed their similarity and differences on the effectiveness of group training for LPP among pregnant women (Table 3).
Meta-analysis
Meta-analysis was done using Review Manager (RevMan 5, Cochrane Collaboration, Oxford, UK). The postintervention data’s were used to obtain the pooled estimate of the effect of intervention. Heterogeneity between trials was assessed using the I2 statistic. Heterogeneity was considered substantial if I2 was greater than 50% and a random effects model applied; otherwise a fixed effects model was used for the analysis. The pooled data for each outcome were reported as weighted mean differences with a 95% confidence interval (CI).
RESULTS
A total of 344 articles were identified from the electronic search, but only 5 RCTs were found to fulfill the inclusion criteria. Included articles were high quality RCTs which their score in PEDro scale above average.
A total of 2,087 pregnant women aged 18 and above with gestational age from 18 to 36 weeks were included in the five studies. Self-reported LPP was used as a common outcome measure for most of the studies (Eggen et al., 2012; Haakstad and Bø, 2015; Mørkved et al., 2007; Stafne et al., 2012). Visual analogue scale was used by three studies (Eggen et al., 2012; Haugland et al., 2006; Mørkved et al., 2007) and two articles used an outcome measure sick leave due to LPP (Mørkved et al., 2007; Stafne et al., 2012).
Pregnant women participated in the experimental group had received starting from educational program on LPP and Ergonomics to different exercises such as aerobics, strengthening and stretching exercises in group once a week and home exercises but the pregnant women from the control group received usual or standard antenatal care.
Effect of group training
The effect of group training on LPP on pregnant women at 36 weeks gestational period was examined by pooling data from four trails which used self-reported LPP (Eggen et al., 2012; Haakstad and Bø, 2015; Mørkved et al., 2007; Stafne et al., 2012) involving 1,159 participants. The mean effect of group training in all the included studies in this meta-analysis favors group training than routine antenatal care for the treatment of LPP among pregnant women (Fig. 1).

Mean difference (95%) of effect of group training versus control group for lumbopelvic pain (LPP) intervention (n=1,159).
From the four studies included significant effect of group training was detected over usual antenatal care or no treatment with P=0.0035 (95% CI, −0.2348 to −0.0044). Heterogeneity between studies was negligible (I2=0.0%) and fixed effect model was used for analysis (Fig. 2).
DISCUSSION
Evidences on the effect of group training on pregnancy induced LPP are very controversial in which a number of studies showed as not effective and few studies suggested as it is effective. Therefore the aim of this review was to decide whether group training is beneficial or not to treat pregnant women who suffered from LPP. The overall result of the trials included in the meta-analysis indicates that group training is significantly effective at reducing LPP after pregnancy. Similarly one study showed that group training can significantly reduce LPP among pregnant women (Mørkved et al., 2007).
On the other hand there are studies which showed that group training has no effect in the treatment of LPP among pregnant women (Eggen et al., 2012; Haakstad and Bø, 2015; Haugland et al., 2006; Stafne et al., 2012). This difference could be due to the differences in the exercises and this systematic review with meta-analysis had taken data from all the studies and brings a new result which showed group training is found to be effective to treat LPP.
Even though all the RCTs concerning group exercise for LPP after pregnancy had taken because there is a scarce of studies in the area, this review was done by two authors with the help of other experts in analysis and in review which can methodologically leads to selection of articles bias, which could be negotiated by third author.
The results of this systematic review proposed that group training reduces LPP significantly better than routine antenatal care for pregnant women suffered from LPP. Group training is very useful to save time and human power especially in resource limited settings. Most of the studies included in this review were used the guidelines of American College of Obstetricians and Gynecologists with modifications according to their setup. Therefore clinical decision making shall be made based on patient’s safety, patient’s preferences and therapist expertise.
ACKNOWLEDGMENTS
We feel very happy to express our special gratitude for staffs from Department of Epidemiology and Biostatistics, University of Gondar for their help in the analysis. We also appreciate Mr. Janakiraman Balamurugan from Department of Physiotherapy, University of Gondar for his support in reviewing and finding appropriate journal for dissemination.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.