Effects of body mass index on foot posture alignment and core stability in a healthy adult population
Article information
Abstract
Foot biomechanics and core stability (CS) play significant roles in the quality of standing and walking. Minor alterations in body composition may influence base support or CS strategies. The aim of this study was to investigate the effect of the body mass index (BMI) on the foot posture index (FPI) and CS in a healthy adult population. A total of 39 healthy adult subjects with a mean age of 24.3±6.4 years and over-weight BMI values between 25 and 29.9 kg/m2 (27.43±6.1 kg/m2) participated in this study. Foot biomechanics were analyzed using the FPI. CS was assessed using a plank test with a time-to-failure trial. The Spearman correlation coefficient indicated a significant correlation between BMI and both the FPI (r=0.504, P=0.001) and CS (r= −0.34, P=0.036). Present study concluded that an overweight BMI influences foot posture alignment and body stability. Consequently, BMI should be considered during rehabilitation management for lower extremity injuries and body balance.
INTRODUCTION
The number of individuals with excessive body weight is rapidly increasing in many countries. In terms of global burden of disease, more than one-third of all adults are currently overweight or obese (Kitahara et al., 2014). Body adiposity has been consistently linked to a greater risk of musculoskeletal pain and injury in the general population (Peltonen et al., 2003), and emerging evidence suggests that even modest increases in body mass index (BMI) are sufficient to induce musculoskeletal pain and difficulties in ambulation (Hulens et al., 2003). Despite the multifactorial nature of musculoskeletal disease, a high BMI has repeatedly emerged as a key and potentially modifiable risk factor in the onset and progression of musculoskeletal disorders that affect the lower limbs, such as knee and hip osteoarthritis (Anandacoomarasamy et al., 2008). Moreover, a higher BMI has profound effects on soft-tissue structures, such as tendons, fascia and cartilage. Obesity is considered a predictor of postural stability, and a high BMI is an important risk factor for geriatric falling (Hue et al., 2007). In addition, the negative consequences of a higher BMI extend well beyond physiological aspects; obese individuals are less efficient and at greater risk for injury than normal-weight individuals in a large number of work-related tasks and daily activities that involve upright standing positions (Berrigan et al., 2006). Such abnormalities associated with increased BMI may influence the core stability (CS) and foot posture index (FPI).
CS has been defined as “the body’s ability to control the trunk in response to internal and external disturbances, including the forces generated from distal body segments as well as from expected or unexpected perturbations” (Zazulak et al., 2007). The CS of the abdominal and pelvic regions plays an important role in lumbar posture control by tonic or postural muscles (Marshall and Murphy, 2005). CS exercises produce significant improvements in the distribution of ground reaction forces and the use of optimized postural adjustments in the direction of a perturbation (Muthukrishnan et al., 2010). Furthermore, preliminary evidence shows that CS training reduces the injury rate (Willson et al., 2005). It is surprising that most CS studies have examined CS training aspects but have not investigated the benefits for normal adults. Despite the widespread use of CS training, the relationship between CS and varying BMI has not been studied. However, it is well known that both CS and the BMI affect the quality and performance of standing body balance and walking.
The FPI is considered a novel, valuable and reliable diagnostic clinical tool to quantify positional variations of the foot. The FPI measures foot posture in three planes and two anatomical segments and take into consideration six assessment criteria. Foot posture alignment deviations, including pronation and supination, may be evaluated using the FPI (Redmond et al., 2006). Body weight has been found to be significantly associated with elevated loading of the foot. Hence, the FPI plays an important role in determining the quality of standing activities, such as standing balance, walking and running. DPT-Work-Power-1eficits in the quality of the foot arch congruity, flexibility and strength have been assumed to disturb foot functions. A previous study showed a strong relationship between foot arch type and injury risk; in particular, high and low foot arches were shown to increase the risk of skeletomuscular injuries (Cowan et al., 1993). Human foot biomechanics vary among healthy individuals and range from low to high arch foot types (Redmond et al., 2008). However, an evaluation of the relationship between the FPI and varying BMI has not been performed. This relationship may influence lower extremity kinematics and contribute to musculoskeletal injuries.
Regardless of whether BMI variations affect the FPI and CS, the elucidation of a possible relationship between an overweight BMI and the FPI and CS is important for developing preventive strategies to improve the quality of life. Hence, the aim of this study was to investigate the correlational effects of BMI variations on the FPI and CS.
MATERIALS AND METHODS
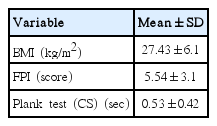
Thirty-nine nonathletic, male university students aged 22–27 years with a mean age of 24.3±6.4 yr, height of 171.96±5.51 cm, weight of 82.9±17.2 kg, BMI between 25 and 29.9 kg/m2 (27.43±6.1 kg/m2) and FPI values between 0 and +10 (5.54±3.1) voluntarily participated in this study. The study exclusion criteria consisted of any sign of foot pain, reduced tactile and thermal foot sensibility, peripheral neuropathy, a history of patellofemoral pain syndrome, plantar fasciitis, back pain, a BMI>30 kg/m2, limb-length discrepancy, anterior or posterior tibialis dysfunction or evidence of a systemic or musculoskeletal disease within the past six months that would affect daily activities.
Foot biomechanics and CS were assessed using the FPI and a plank test, respectively. All the protocols were approved by the ethical committee on human research and followed ethical standards.
Assessment procedures
Body mass index
The World Health Organization classifies individuals into three groups based on body mass: normal (BMI<25 kg/m2), overweight (BMI, 25–30 kg/m2) and obese (BMI>30 kg/m2) (World Health Organization, 1997). The heights of participants were measured using a stadiometer (Invicta Stadiometer, Invicta, London, UK) with a calibrated analog scale. The weights of participants were measured with a scale (Breuer electronics scale) with a precision of 0.01 kg. During the measurements, the subjects had bare feet and wore only underwear, and the measurements were recorded in kg. The height of each subject was measured in an upright position with a metal bar that was fixed to a sensitive bascule. Special attention was given to ensure that the subject’s body was fully upright and their mandible was parallel to the ground. Height values were recorded in cm. The BMI, which is a useful measurement for evaluating excess body fat, was calculated as the body weight divided by the square of the height (kg/m2) for each individual (de Oliveira Pinheiro et al., 2004).
Core stability
The CS was measured by anterior core muscular-endurance testing, which consisted of a single time-to-failure trial in a timed prone bridge position (McGill et al., 1999). The investigator timed the trial using a digital hand-held stopwatch (model Triathlon; Timex Group USA, Middlebury, CT, USA). For each test, subjects were given verbal instructions on test positions and a visual example and were asked to hold the position for as long as possible. As soon as the subject was in the correct position, the stopwatch was started. The test was terminated when the subject could no longer hold the position. All single blinded tests were performed under the supervision of the authors to increase interrater reliability. To improve the internal consistency or intrarater reliability, all tests were performed 3 times, and the mean values were recorded. A 5-min rest period was provided between the CS and FPI testing sessions, and the order of testing was counterbalanced to control for fatigue effects.
Foot posture index
The biomechanical assessments of the foot were conducted by the same assessor using the FPI, as described by Redmond et al. (2006). This assay consisted of summing the values obtained for six assessment criteria: FPI-I, talar head palpation; FPI-II, comparison of the curves above and below the lateral ankle malleolus; FPI-III, calcaneal frontal plane position; FPI-IV, prominence in the region of the talonavicular joint; FPI-V, congruence of the medial longitudinal arch; and FPI-VI, abduction/adduction of the forefoot on the rear foot. Each criterion was scored using whole numbers ranging from −2 to +2; thus, the total score ranged from −12 (indicating maximal supination) to +12 (indicating maximal pronation). The reported intertester reliability of the FPI ranges from an intraclass correlation coefficient of 0.62 to 0.91, whereas the intratester reliability ranges from 0.81 to 0.91. The FPI has been shown to be a valid measure of foot posture and is associated with the midstance position of the foot during walking (Redmond et al., 2006).
RESULTS
The SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA) was used for data analysis. The values are reported as the mean±standard deviation (Table 1). The correlations between the variables were assessed using Spearman correlation coefficient.
The results of the current study indicate a significant association between varying BMI and the FPI (r=0.5, P=0.001) and CS (r= −0.34, P=0.036) (Table 2) in healthy subjects. This observation indicates that an overweight BMI may have an effect on variation of the FPI and CS. Thus, the BMI may be an important variable that must be considered during lower extremity rehabilitation.
DISCUSSION
The aim of this study was to examine the effect of an overweight BMI on the FPI and CS. Our findings indicate that an overweight BMI influences the FPI and CS. These findings are consistent with a previous study, which observed that obese women tended to present with flatter feet, and obese men tended to present with more pronated feet (Aurichio et al., 2011). Indeed, it is believed that obesity exerts an abnormal influence on the structure of the foot (Wearing et al., 2012).
One possible explanation for the negative relationship between an increasing BMI and the FPI is that excess bodyweight leads to greater mechanical loading of the foot. It has been suggested that fat mass may be the cause of the outward appearance of a “flat” foot in obese individuals (Wearing et al., 2012). Body weight has been found to be significantly associated with elevated loading of the foot, particularly the forefoot and midfoot, which suggests that obesity increases the stresses applied to the foot directly via increased body weight and indirectly via alterations to the foot structure, i.e., a relatively pronated foot posture (Butterworth et al., 2014). The findings from our study are the first to take into account varying BMI and changes in the FPI.
Interestingly, our biomechanical assessment of the FPI indicated that individuals with an overweight BMI tended to have flat feet. Accordingly, a higher prevalence of obesity has been observed in individuals with flat feet (Wearing et al., 2006), which could be due to the previous observation that a more convex talonavicular prominence and forefoot abduction relative to the rear of the foot are present in individuals with flat feet (Aurichio et al., 2011). The present findings are supported by Hamstra-Wright et al. (2015), who indicated that an increased BMI and changes in foot posture must be considered to prevent and treat medial tibial stress syndrome. Thus, our findings also suggest that an increase in body mass may impact the maintenance of the longitudinal arch, i.e., in heavier individuals, the arch drops. Furthermore, an altered alignment of the talonavicular joint motion in individuals with flat feet indicates impaired midfoot function (Kothari et al., 2014), and motions of the navicular bone in the transverse and sagittal planes are important to consider when evaluating foot function, as shown for the FPI in our study.
It is known that adipose tissue accumulates at the abdominal region in obese individuals. Moreover, it is interesting to note that the rectus abdominal muscle shows the greatest fatty infiltration, followed by the lateral abdominal muscle and erector spinae, in overweight and obese individuals (Ryan and Harduarsingh-Permaul, 2014). These higher levels of intramuscular fat have been associated with reduced functional capacity in healthy older adults (Hicks et al., 2005). Additionally, the activation of the external oblique muscle is higher than that of other core muscles in the prone bridging position regardless of the stability of the support surface (Imai et al., 2010; Garber et al., 2011). Furthermore, an increase in the activation levels of the external oblique and the rectus abdominal muscles during the prone bridging position has also been observed (Lehman et al., 2005).
Spinal instability is associated with reduced strength and endurance of the core musculature and altered recruitment of these muscles (Hibbs et al., 2008). Consistent with these findings, decreased muscle activity could be a possible explanation for the correlation between a higher BMI and CS.
The present study emphasizes the importance of the correlation between BMI and CS as CS is critical for the transfer of energy from the larger torso to the smaller extremities during many sports and activities (Tse et al., 2005). Therefore, it is believed that if the extremities are strong and the core is weak, the decrease in muscular summation through the core will result in less force production and inefficient movement patterns. To maintain stability of the core, the body must integrate sensory, motor-processing, and biomechanical strategies coupled with learned responses and the ability to anticipate change (Comerford and Mottram, 2001). Thus, the body must control the trunk in response to internal and external perturbations, which include forces generated by the distal extremities and expected/unexpected challenges to stability (Borghuis et al., 2008). Anticipatory postural adjustments of the core are determined by preprogrammed muscle activations (Kibler et al., 2006). Muscle activation patterns in response to rapid arm movements have been demonstrated to begin in the lower extremities and proceed upward through the trunk and to the arms (Cordo and Nashner, 1982); these postural adjustments allow the body to increase proximal stability and enable distal mobility.
Our study results are consistent with previous studies showing that the endurance of core muscles is correlated with a reduced back endurance test (Fogelholm et al., 2006; Kankaanpää et al., 1998). Similarly, an inverse relationship between the BMI and endurance time during sustained isometric grip contractions at 30% of maximum strength has been reported (Eksioglu, 2011). Moreover, the effects on muscle fatigue due to excess weight have produced similar reductions in endurance times and rates of strength loss in younger individuals (Cavuoto and Nussbaum, 2013; Maffiuletti et al., 2007). Furthermore, obese individuals have reported greater discomfort during physical exertion than their lean counterparts (Cavuoto and Nussbaum, 2013). Our study subjects were in the borderline obesity range, which indicates that the observations from previous studies may support the correlation between a higher BMI and CS.
Most studies have examined the training aspects of CS, and few studies have investigated the benefits of CS in normal adults. Despite having an overweight BMI, the participants of this study were considered healthy subjects and were not limited in their functional activities. Furthermore, the BMI is the most commonly used general indicator of adiposity but does not distinguish between fat and lean body masses (Sun et al., 2010). Additional confounding factors of this study include the small sample size and the single data collection time point. These factors may have limited the study to a relatively narrow window of different durations of obesity and its effects on the FPI and CS. Further investigations should be conducted to determine the role of each FPI component.
The present study revealed a strong correlation between a higher BMI and the FPI and CS. These study variables should be considered during preventive rehabilitation. During physical treatment and rehabilitation, the identification of a poor FPI and a lack of CS are considered risk factors for lower extremity musculoskeletal injuries (Wilkerson and Colston, 2015; Hamstra-Wright et al., 2015). Thus, the BMI should be considered an important variable and should be given sufficient attention during lower extremity rehabilitation. Proper therapeutic management supported by diet counseling and weight reduction programs will facilitate an effective prevention and rehabilitation program.
ACKNOWLEDGMENTS
The authors would like to extend their appreciation to the Deanship of Research, Research Center, College of Applied Medical Sciences at King Saud University for constructive scientific support during this research.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.