The effects of objectively measured physical activity and fitness on fear of falling among Korean older women
Article information
Abstract
We examined the effects of objectively measured physical activity (PA) and physical fitness (PF) on fear of falling (FOF) among older adults. The subjects were 94 Korean females aged 65–79. PA was measured with accelerometers, PF with the senior fitness test and FOF with the Korean Survey of Activities and Fear of Falling in the Elderly. With the subjects’ age, number of chronic conditions, and history of falls included as correction factors, a multiple regression analysis showed that PA (P=0.016) and agility/dynamic balance measured by the 8-foot up-and-go test (UNG) (P=0.001) significantly influenced FOF. The FOF of the slowest UNG quartile was significantly higher than those of other groups (P=0.002). This study concludes that among female older adults agility/dynamic balance as measured by UNG is the main factor impacting FOF and individuals with markedly low UNG tend to have high FOF.
INTRODUCTION
Physical activity (PA) and physical fitness (PF) levels of older adults tend to decline with aging (Milanović et al., 2013). Decreased PA and PF can lead to a wide range of health issues. One of these issues is fear of falling (FOF). FOF is one of the risk factors involved in falling (Cumming et al., 2000; Friedman et al., 2002) and it can exert negative effects on older adults’ physical functioning (Brouwer et al., 2004; Deshpande et al., 2008), social relationships (Scheffer et al., 2008), and quality of life (Lach, 2005).
A number of studies of older adults have shown PA and FOF to be related (Murphy et al., 2003; Schepens et al., 2012). However, most of these studies used self-report to measure PA. The accuracy of subjective assessment in older adults could be affected by possible lessening of cognitive capabilities due to aging and it is difficult to translate self-reported data into quantified data. Therefore, the use of objective, rather than subjective, instruments in research on PA with older adults can be expected to increase reliability of measurement. In one study employing objective measurements (Hornyak et al., 2013), FOF was found to be significantly associated with total daily activity, although the relationship was weak (r=−0.26, P=0.02). One reason for the weakness of this relationship could be the inclusion of both sexes as subjects, because it has been shown that there are differences between men and women in PA patterns (Sun et al., 2013) as well in levels of FOF (Scheffer et al., 2008). Female older adults have been found to have lower PA levels and higher FOF levels than those of male older adults (Scheffer et al., 2008; Sun et al., 2013).
In addition to PA, PF has also been found to influence FOF. Among the PF factors, balance and strength have often been shown to be related to FOF in older adults (Austin et al., 2007; Brouwer et al., 2004; Clemson et al., 2012; Gillespie and Friedman, 2007; Lach, 2005; Park et al., 2014; Toraman and Yildirim, 2010). However, more various fitness factors, including balance, strength, coordination, endurance, and flexibility, are generally recommended for or included in intervention programs for fall prevention or FOF reduction (Gillespie and Friedman, 2007; Panel on Prevention of Falls in Older Persons, American Geriatrics Society and British Geriatrics Society, 2011; Zijlstra et al., 2007). Therefore, we tried to clarify main PF factors related to FOF in Korean older women for the establishment of efficient intervention program.
The purpose of this study was to investigate the effects of PA and PF on FOF in Korean female older adults, with the expectation that our research might contribute to the development of effective intervention programs designed to decrease FOF and the occurrence of falling. In order to base the findings on objective data, we used accelerometers to measure PA and the senior fitness test (SFT) to measure PF.
MATERIALS AND METHODS
Participants
The subjects of this study were Korean female older adults who volunteered to participate in the research in response to notices posted in Seoul at four senior citizen’s centers, two public health centers, and two churches. Given the nature of the research, volunteers in the following categories were excluded as subjects: those with physical conditions limiting PA, such as muscular or bone injuries, serious cardiovascular diseases, strokes, and Parkinson disease; those with mental illnesses that hindered normal communication; and those requiring assistance for PA. There were 125 remaining subjects.
The research plans and the procedures for obtaining consent from the subjects had been approved by the Ewha Womans University Institutional Review Board. Of the group of 125 subjects, it was necessary to exclude 27 people due to a lack of time to measure physical activities and because of other errors, and 4 additional people due to errors in completing the questionnaire. The ages of the final 94 subjects ranged from 65 to 79. Other characteristics of the subjects are presented in Table 1.
Predisposing factors
Information on demographic variables, health status, and previous history of falls were gathered by trained researchers using a questionnaire. Age, number of chronic conditions, and history of falls within the preceding year were used as correction factors in the subsequent analyses.
Fear of falling
This study utilized the Korean version of the Survey of Activities and Fear of Falling in the Elderly (K-SAFFE). K-SAFFE is one of the well-known FOF scales (Bladh et al., 2013). The Korean version of this survey consists of eight items of four-level Likert scales, where a higher number indicates greater FOF. The internal consistency (Cronbach alpha) of the survey was found to be 0.675 for easy activities and 0.734 for difficult tasks.
Physical activity
An individual’s PA was measured using a Fitmeter (Fit.Life, Seoul, Korea), a 3-axial accelerometer. The Fitmeter was designed to present acceleration values directly. This study assumed a constant gravitational acceleration and calculated the signal vector magnitude (SVM) to aggregate each axis’ acceleration values according to the following formula: SVM=(ax2+ ay2+ az2)1/2
A high correlation (r=0.947) and high explanatory power (R2=0.897) were observed between the SVM of the Fitmeter and the count-based values measured by the ActiGraph (Model wGT3x-BT, Pensacola, FL, USA). In addition, a high correlation (r=0.821) had been previously found between SVM value and oxygen consumption (Kim et al., 2014).
The sampling interval was set at 10 sec, and the subjects were requested to wear the device for seven consecutive days, from the time of getting out of bed in the morning until going to bed at night, except during activities with water, such as showering or swimming. The monitor was worn above the right iliac spine and fastened with an elastic band. After wearing the device for a week, the subjects returned it to the researchers, who then downloaded the data with the Fitmeter software. A respondent’s data were only used if there were over 5 days in total for which data from the monitor indicated that it had been worn for over 10 hr throughout the day. From the PA data gathered by the accelerometers, we used SVM values as the variable representing PA level.
Physical fitness
To assess subjects’ PF, the study employed the SFT (Rikli and Jones, 2012). An individual’s general endurance was measured by means of the 2-min step test, upper/lower-body strength by the arm curl test and the chair stand test, upper/lower-body flexibility by the back scratch test and the chair sit and reach (CSR) test, and agility/dynamic balance by the 8-foot (244 cm) up-and-go (UNG) test. Among the SFT items, the 6-min walk was excluded due to space constraints; and 2-kg dumbbells were used for the arm curl test instead of 2.3-kg weights. Before participating in the SFT, the subjects performed stretching exercises for 5 min.
Data analysis
The statistical analyses of data were performed using SAS 9.3 (SAS Institute Inc., Cary, NC, USA). Table 1 shows the mean and standard deviation of each variable. Pearson correlation analysis was carried out to examine PA/FOF and PF/FOF relationships. Multiple regression analyses were then conducted to investigate the influences of PA on FOF and PF on FOF. Both analyses included the correction factors of age, the number of chronic conditions, and falling within the preceding year. The statistical power was calculated as 0.445, a somewhat low figure.
The participants were divided into quartile groups based on UNG time, which had the strongest impact on FOF in the regression analysis. The levels of FOF were then compared among the quartile groups using a one-way analysis of variance (ANOVA), followed by Tukey post hoc test. The level of significance for each statistical analysis was set at α=0.05.
RESULTS
The 94 Korean older women whose data were analyzed for this study had a mean of 4.1±2.4 chronic conditions and 12 respondents (12.8%) reported a fall in the previous year. The participants’ FOF levels, measured by the K-SAFFE, had a mean score of 12.9±3.9, ranging from 8 to 32 across the total of 8 questions.
The level of PA and most of the PF measurements showed a significant correlation with FOF; the exception was the CSR test, which is an indicator of flexibility of the trunk and lower extremities (Table 2).
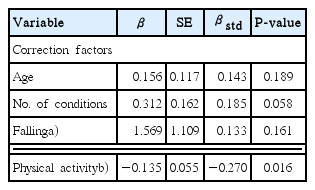
The level of PA had a statistically significant but weak impact on FOF (standardized β [βstd]=−0.270, P=0.016), while the number of chronic conditions was nearly significant (βstd=0.185, P=0.058) (Table 3). The explanatory power of the regression model was 19.6%.
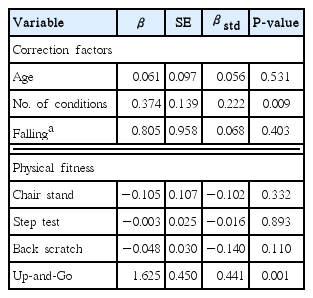
UNG measurements (βstd=0.441, P=0.001) and the correction factor of number of chronic conditions (βstd=0.222, P=0.009) affected FOF significantly (Table 4). The explanatory power of this regression model was 41.6%.
Table 5 displays the result of a one-way ANOVA with FOF as the dependent variable, for the quartile groups formed on the basis of UNG time, the most influential PF variable in the regression analysis. An application of Tukey post hoc test showed the FOF level of quartile 4 (G4) to be significantly higher than those of quartiles 1 (G1), 2 (G2), and 3 (G3).
DISCUSSION
Various intervention programs designed to modify older adults’ lifestyles have been implemented in an attempt to decrease FOF and the risk of falling, taking into account PA and PF. To increase the effectiveness of such programs, it is important to clarify the relationships of PA and PF with FOF and to determine the critical factors influencing FOF.
In this study, PA and most of the PF measurements except CSR test were found to have significant correlations with FOF. Logistic regression analysis, which included age, number of chronic conditions, and experience of falling as correction factors, showed that both PA and the UNG time significantly affected FOF. The correlation between PA and FOF (r=−0.402) was stronger than that in the study of Hornyak et al. (2013), which reported a weak correlation (r=−0.26) between PA measured by accelerometers and FOF assessed by SAFFE. The higher correlation between PA and FOF in our study might be due in part to the homogeneity in sex of our subjects; Hornyak et al. (2013) included both females and males as subjects. However, in our multiple regression analysis, the effect of PA on FOF was not particularly strong (βstd=−0.270, P=0.016) and the explanatory power was low (adjR2=0.196). These results contrast with those of Murphy et al. (2003), in which the relative risk of a “sedentary lifestyle” for the development of FOF was even higher than the relative risks of older age (80+) and visual impairment. It may be the case that a very low level of PA might play a strong role in the development of FOF (Bruce et al., 2002; Murphy et al., 2003; Schepens et al., 2012). In addition, differences between our study and previous studies in the PA measurement tools used and PA variables investigated may in part explain differences in results regarding the relationship between PA and FOF.
As for PF, agility/dynamic balance, measured by the UNG test, was found to be the most important factor related to FOF, as indicated by logistic regression analysis. The UNG test and the timed chair stand test have been often recommended as tools for assessment of mobility and risk of falling in older adults (Dai et al., 2012; Panel on Prevention of Falls in Older Persons, American Geriatrics Society and British Geriatrics Society, 2011). Compared to other fitness tests, including the timed chair stand, the UNG test is unique in its dynamic, multifaceted nature. This one test, composed of various movements (standing, walking, turning, and sitting), evaluates many aspects of physical functioning, such as mobility, agility, and balance. These characteristics of the UNG test seem to make it an excellent instrument for assessing general mobility and for detecting the effect of relatively subtle psychological factors such as FOF.
In our study, the FOF of older women whose UNG time was the slowest (quartile 4) was significantly higher than the FOF of those in quartiles 1, 2, and 3. This is in line with the findings of Austin et al. (2007), who reported that obesity and slower timed UNG (quintiles 4 and 5) predicted new onset of FOF. The results of both studies suggest that older people whose agility/dynamic balance or mobility is markedly low may have greater FOF. On the basis of these findings, we suggest that exercise programs designed to decrease FOF should focus on improving agility/dynamic balance.
ACKNOWLEDGMENTS
This study was supported by the Health Promotion Fund, Ministry of Health & Welfare, Republic of Korea (General Research, 12–26).
Notes
CONCLICT OF INTEREST
The authors declare no conflict of interest.