Joint predictability of physical activity and body weight status on health-related quality of life of patients with hypertension
Article information
Abstract
This study investigated the predictability of physical activity (PA) and body weight status (BWS) on health-related quality of life (HRQoL) of patients with hypertension. A cross-sectional study involved 250 patients with hypertension (≥140/90≤179/109 mmHg) selected from government hospitals in Osun State, Nigeria. Purposive sampling technique was used to select participants. Socio-demographic characteristics and cardiovascular parameters were recorded. PA and HRQoL were assessed using the International Physical Activity Questionnaire and Short Form health survey questionnaire respectively. Sufficient PA equals ≥150 min/wk while BWS was defined using body mass index classification. Data were analyzed using descriptive and inferential statistics. Alpha level was set at P<0.05. Of all participants, 63.6% reported sufficient PA and 78.4% was either overweight or obese. The HRQoL of participants become poorer in all domains with higher body weight. The HRQoL including role limitation due to physical health (RLdPhp) and emotional problems (RLdEmp) had worst scores. Participants in the categories of normal and overweight/obese with sufficient PA demonstrated higher (better) HRQoL in all domains than those with insufficient PA (P<0.05). When adjusted for body weight, significant differences were found in all domains of HRQoL except in RLdPhp, RldEmp, and bodily pain (P>0.05). There were significant correlations between PA and all domains of HRQoL except in RldEmp, emotional well-being and bodily pain (P>0.05). Regression models established PA as a significant predictor of HRQoL. Sufficient PA is a better predictor of HRQoL among patients with hypertension irrespective of BWS. Regular PA is recommended for improving HRQoL among patients with hypertension.
INTRODUCTION
The World Health Organization (WHO) projects that over the next 10 years Africa will experience the largest increase in death rates from cardiovascular disease (CVD) as a result of increasing prevalence of hypertension (World Health Organization [WHO], 2011). Africa, a continent of 53 countries with one billion population is not only threatened by a huge burden of infectious diseases but also bears a considerable proportion of the world’s CVD burden due to high prevalence of hypertension (Hajjar et al., 2006; WHO, 2005a). Unfortunately, the dearth of valid epidemiological data to describe the magnitude of hypertension preponderance is a significant shortcoming in the region. Nonetheless, hypertension has been identified as an important risk factor for CVD and is portending an unimaginable public health disasters for sub-Sahara Africa unless urgent actions are taken (BeLue et al., 2009; van de Vijver et al., 2013).
Hypertension is associated with stroke, hypertensive heart disease, cardiac arrest, myocardial infarction, congestive heart and kidney failures (Alberts et al., 2005; Bygbjerg, 2012). There are known myriad of risk factors for hypertension including but not limited to advancing age, rapid urbanization, series of lifestyle changes which include poor dietary habits, heavy alcohol abuse, cigarette smoking, stress, poor socio-economic status, obesity and physical inactivity, thus contributing to high prevalence of hypertension (Chobanian et al., 2003; Kearney et al., 2005). Evidence from epidemiological studies have shown that individuals with low physical activity (PA) coupled with overweight/obesity were almost twice more likely than those with normal weight to be at higher risk of CVD event (Sobngwi et al., 2002; Wang et al., 2006). Indeed, physical inactivity has been identified as the fourth risk factor for death but is rapidly advancing to become the leading risk for global morbidity and mortality (Bull and Bauman, 2011; WHO, 2009).
In the recent time, epidemiological studies have shown that hypertension and obesity are important factors contributing to the impairment of health-related quality of life (HRQoL) (Ogunlana et al., 2009; Pan et al., 2011). Despite the fact that mild to moderate hypertension is generally asymptomatic, its detection, and diagnosis may negatively impact on HRQoL of individuals with hypertension (Maruf et al., 2013). Although evidence from interventional studies have shown that pharmacological treatment of hypertension helps to lower blood pressure and reduce target organ damage (Familoni et al., 2004; Salako et al., 2004), successful treatment rate of hypertension is still below optimal level (Awotidebe et al., 2014; Pescatello et al., 2004). Notably, factors contributing to unsuccessful treatment of hypertension and poor HRQoL include adverse effect of antihypertensive medications and cost, labeling or beliefs and attitudes about illness and treatment (Maruf et al., 2013; Ogunlana et al., 2009). Fortunately, substantial evidence from several studies have shown that participation in regular and sufficient PA is associated with reduction in blood pressure, and reduction in CVD risk (Maruf et al., 2013; Pan et al., 2011; Tsai et al., 2004; Warburton et al., 2006).
There is no doubt that reduction in body weight lowers blood pressure and subsequently improves HRQoL (Pan et al., 2011; Tsai et al., 2004). However, achieving an optimal body weight is an enormous challenge for overweight or obese individuals presenting with or without hypertension. Nevertheless, it is not known whether regular engagement in sufficient PA with an unchanged body weight status translates to satisfying HRQoL among patients with hypertension. Understanding the import of HRQoL as a health outcome could help to capture a person’s perception of overall health status and as well help to inform decisions on resource allocation for effective management of hypertension (WHO, 2005b).
In view of this, many health authorities have advocated the adoption of lifestyle modifications including regular and sufficient PA and body weight control programmes as nonpharmacological approaches for effective hypertension control and satisfying HRQoL (Chobanian et al., 2003; WHO, 2003). However, the extent to which both PA and body weight status jointly impact on HRQoL of patients with hypertension remains poorly understood. Furthermore, a few studies have examined the combined effect of PA and body weight status on HRQoL of patients with hypertension in Nigeria. Hence, the purpose of this study was to investigate the joint predictability of PA and body weight status on HRQoL of Nigerian patients with mild to moderate hypertension
MATERIALS AND METHODS
Participants and locations
Participants for this study were individuals with mild to moderate hypertension (≥140/90 ≤179/109 mmHg) receiving treatment at selected government hospitals in Osun State, Nigeria. Purposive sampling technique was used to recruit participants from Ife Hospital Unit, Ile - Ife and Wesley Guild Hospital, Ilesha, both belonging to the Obafemi Awolowo University Teaching Hospitals Complex and State Government Hospital, Asubiaro, Osogbo, Osun State, Nigeria. Eligibility for inclusion were patients with clinical diagnosis of mild to moderate hypertension, receiving treatment at the Consultant Out-Patient Department, Cardiac Care Units of the selected government hospitals, self-reported optimal blood pressure control and regular use of prescribed antihypertensive medications. They were excluded from the study if presented with uncontrolled hypertension (≥180/110 mmHg), unstable angina or severe medical co-morbidities such as uncontrolled type 2 diabetes, asthma, and previous history of myocardial infarction or neurological conditions including stroke. They were also excluded if presented with difficulty in understanding or inability to complete the questionnaires due to dementia.
The sample size for this study was based on a sample size formula for cross-sectional survey. The sample size was calculated using the computer program for epidemiologists (PEPI), version 3.01, employing the formula for estimating sample size for single proportion as described by Abramson and Gahlinger (2001). The following parameters were considered to arrive at a minimum sample size for this study; a prevalence rate of 36.6% of hypertension was reported among elderly individuals in Ile - Ife using the 140/90 mmHg cutoff point (Adedoyin et al., 2008). Furthermore, a precision margin of 5% with a standard normal deviate of 1.96 at 95% confidence interval was chosen. Thereafter, a maximal allowable difference from the true proportion of 5% (0.5) was considered and eventually, a sample size of 198 was estimated. However, the sample size was increased to 250 to allow for 10%–20% incomplete response or missing data with the view to improving the validity of data.
Protocol design
This cross-sectional study involved patients with mild to moderate hypertension from selected government hospitals in Osun State, Nigeria. Ethical approval for the study was obtained from the Health Research and Ethics Committee of the Institute of Public Health (IPHOAU/12/421), Obafemi Awolowo University, Ile - Ife, Osun State, Nigeria. Permission to recruit prospective participants was sought and obtained from various Heads/Consultant-in-Charge of the Cardiac Care Units of the selected hospitals after explaining the purpose of study. Furthermore, the purpose of the study was explained to the participants and written informed consent was obtained. Socio-demographic characteristics including age, sex, occupation and monthly income were recorded.
Assessment of anthropometric characteristics and cardiovascular parameters
Anthropometric measures including current body weight and height were measured using standard procedures. Furthermore, body mass index (BMI) (weight [kg]/height [m2]) was calculated and classified as underweight (<18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2) and obese (>30 kg/m2) (WHO, 1995). Body weight status (BWS) was defined as BMI that remains the same (unchanged) in the last 3 months. Cardiovascular parameters including systolic blood pressure (SBP), diastolic blood pressure and heart rate (HR) were all measured in sitting position after rested for about 10 min of arriving the venue of the study. Thereafter, PA level and HRQoL were assessed using the Short-Form International Physical Activity Questionnaire and Short Form-36 (SF-36) Health Survey Questionnaire respectively.
Assessment of PA level
The Short Form version of the International Physical Activity Questionnaire (IPAQ) was used to assess PA in this study. The questionnaire has an acceptable test-retest reliability and criterion validity in Nigerian population (Oyeyemi et al., 2011). Participants were asked the number of days they did vigorous PA, moderate PA excluding walking, then also walking, as well as the number of hours and minutes per day they did the three kinds of activities in the last 7 days respectively. The PA included any PA they did: (a) at work, (b) as part of house and yard work, (c) to get from place to place, and (d) in spare time for recreation, exercise or sport, but with no information on frequency and duration for these separate domains. Respective total hours for vigorous PA, moderate PA and walking were calculated.
A metabolic equivalent (MET)-hr was derived by multiplying the respective total hours with the MET value of vigorous PA (MET=8.0), moderate PA (MET=4.0) and walking (MET=3.3), and then adding all three (IPAQ 2005). PA levels were initially classified as low, moderate, or high intensity, defined by the IPAQ core group (http://www.ipaq.ki.se) as follows: Low—no activity or some activity reported, but not enough to satisfy the requirements of the other activity categories; Moderate—any of the following 3 criteria: (a) 3 or more days of vigorous-intensity activity for at least 20 min per day, (b) 5 or more days of moderate intensity activity or waking for at least 30 min per day, or (c) 5 or more days of any combination of walking, moderate intensity, or vigorous-intensity activities achieving a minimum of 600 MET-minutes per week; High—either of the following 2 criteria: (a) 3 or more days of vigorous-intensity activity accumulating at least 1,500 MET-minutes per week or (b) 7 days of any combination of walking or moderate- or vigorous intensity activities achieving a minimum of 3,000 MET-minutes per week. These 3 groups were then recategorized as sufficient or insufficient PA. Sufficient PA group included participants in the moderate- or high intensity categories who met the WHO PA recommendation. According to the new WHO global standard, satisfying the recommendations for healthy PA was defined as engaging in at least 150 min of moderate-intensity activity per week, 75 min of vigorous-intensity activity per week, or an equivalent combination of moderate- and vigorous-intensity activity (WHO, 2010).
Assessment of HRQoL
The HRQoL of participants was assessed using the Medical Outcomes Study Short Form-36 (SF-36) Health Survey Questionnaire. The SF-36 item is one of the most widely used generic measures of HRQoL with good psychometric properties and substantial data on its applicability in clinical and research settings in Africa (Ekwunife et al., 2011; Ware and Gandek, 1998). The 36-items health survey tool assesses eight health dimensions referred to as subscales namely physical functioning (10 items), role limitations due to physical problems (RLdPhp: 4 items), role limitation due to emotional problems (RLdEmp: 3 items), bodily pain (2 items), general health (5 items), vitality (4 items), social functioning (2 items), and emotional well-being (5 items). These subscales’ scores were summarized into physical and mental composite summaries (physical composite summary [PCS] & mental composite summary [MCS]) domains. Individual SF-36 items were recoded, summed and transformed. The health concepts described by the SF-36 range in score from 0–100, with higher scores indicating higher levels of function or better health (Ware and Gandek, 1998). The cultural adaptation and psychometric properties of SF-36 in Yoruba language showed that the convergent validity was satisfactory, ranging from 0.421 to 0.907, discriminant validity was also satisfactory except for item ‘1.’ The intraclass coefficient for the test-retest reliability ranges between 0.636 and 0.843 for scales and 0.783 and 0.851 for domains (Mbada et al., 2015).
Statistical analyses
Descriptive statistics of frequency, percentage, mean and standard deviation were used to summarize data. Physical characteristics and PA (MET-min/wk) level of participants were compared between genders using t-test while chi-square test of association was used for the categorical variables. Participants’ HRQoL with sufficient PA and insufficient PA with respect to normal weight, overweight and obese were also evaluated using independent t-test. Pearson moment correlation test was used to determine the relationships between HRQoL subscales and each of age, BMI and PA level (MET-min/wk). Multiple linear regression analyses were conducted by block to establish the important predictors of HRQoL among patients with hypertension. All subscales of HRQoL were chosen as outcome variables while age, sex, PA, and BMI were used as predictor variables for the models. The demographic variables were entered in the first block, PA was entered in the second block and BMI was entered in the third block. Alpha level was set at P<0.05. The IBM SPSS Statistics ver. 19.0 (IBM Co., Armonk, NY, USA) was used to perform statistical analyses.
RESULTS
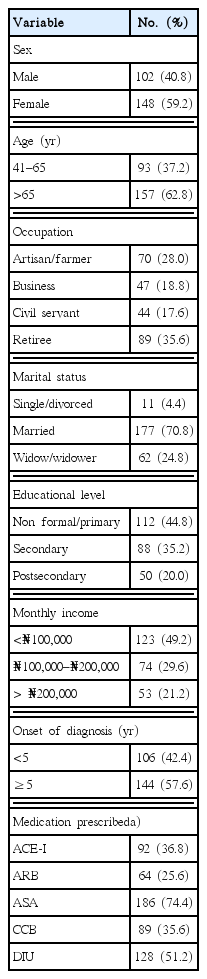
Table 1 shows socio-demographic characteristics and clinical profiles of all participants. There were more female than male participants and about two-thirds, 62.8% of participants were older than 65 years. More than half, 57.6% of participants had greater than 5 years onset of diagnosis of hypertension. A majority, 74.4% of the participants were on low dose Aspirin in combination with antihypertensive medications. The mean age of all participants was 61.6±10.2 years. All participants were comparable in all physical characteristics and cardiovascular parameters (P>0.05), but significant differences were found in BMI and SBP between sexes (P<0.05). Furthermore, no significant difference was found in PA (MET-min/wk) (P>0.05). About 63.6% of participants reported sufficient PA while 78.4% was either overweight or obese (Table 2). Table 3 shows comparison of HRQoL of patients with hypertension by PA and body weight status. The results show that all domains of HRQoL of participants with sufficient PA were significantly higher (better) than those with insufficient PA except the bodily pain domain. Among participants with overweight/obese, the HRQoL decreases in all domains with increasing body weight, however, significant difference was found in bodily pain domain (P<0.05). Furthermore, two subscales of the HRQoL including role limitation due to physical health problems (RLdPhp) and emotional problem (RLdEmp) had the worst scores (Table 3).
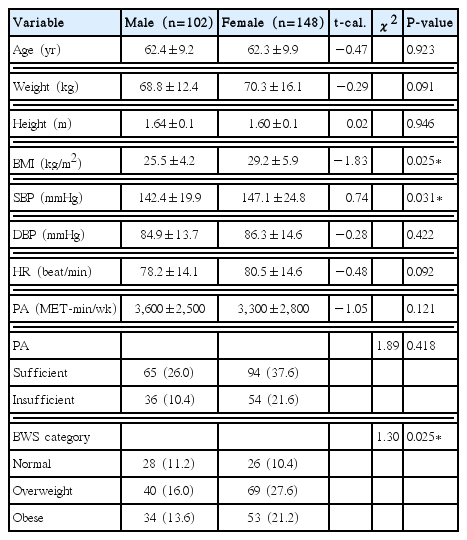
Comparison of anthropometric characteristics, cardiovascular parameters, physical activity and body weight status by sex
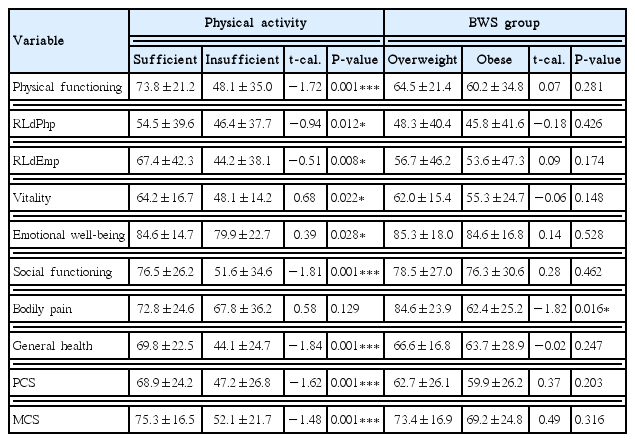
Comparison of health-related quality of life of patients with hypertension by physical activity and body weight status
Table 4 shows comparison of HRQoL of patients with hypertension with respect to sufficient and insufficient PA adjusted for body weight. When adjusted for body weight, the impact of PA was more pronounced on HRQoL. Among participants who reported sufficient PA and belonged to either normal weight or overweight/obese category, the HRQoL scores were higher (better) in all domains including PCS and MCS than those with insufficient. Among normal body weight category, significant differences were found in HRQoL between those with sufficient and insufficient PA; physical functioning (t=−1.72, P=0.001), vitality (t=0.68, P=0.022), emotional well-being (t=0.39, P=0.028), social functioning (t=−1.81, P=0.001), general health (t=−1.84, P=0.001), PCS (t=−1.62, P=0.001), and MCS (t=−1.48, P= 0.001). Furthermore, among participants with overweight and obese categories, significant differences were found in all domains of HRQoL between participants with sufficient PA and insufficient PA except in social functioning and bodily pain (P>0.05).
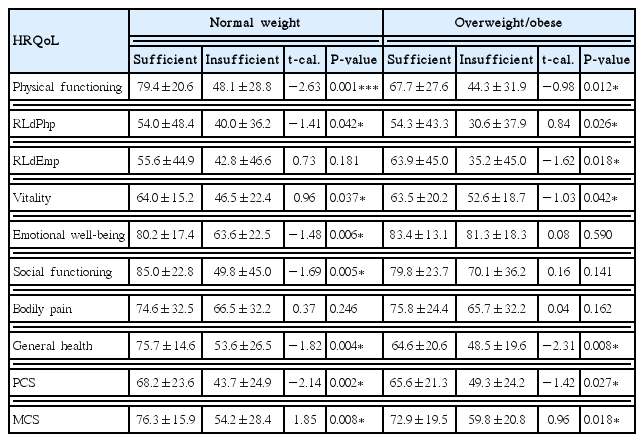
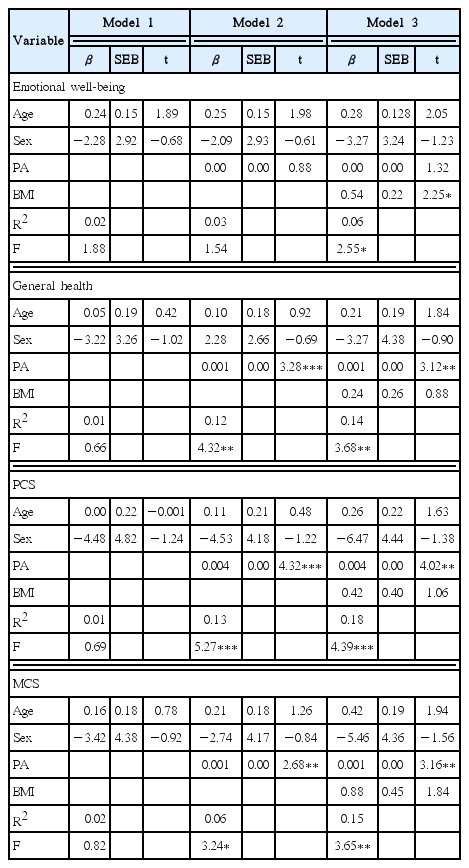
Comparison of HRQoL of patients with hypertension with respect to sufficient and insufficient PA adjusted for body weight status
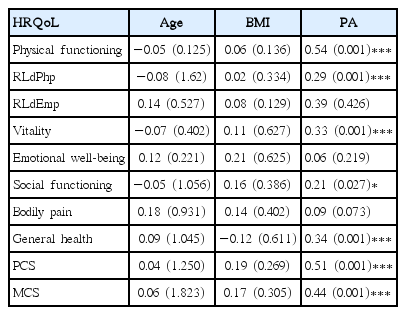
Table 5 shows the relationships between HRQoL domains, age, BMI and PA (MET-min/wk). The results showed that PA demonstrated significant correlations with HRQoL in all domains including both PCS and MCS (P<0.05). However, there were no significant correlations between PA and each of RLdEmp, emotional well-being and bodily pain domains (P>0.05). Furthermore, the relationships between HRQoL, age and BMI showed no significant correlation (P>0.05). Tables 6 and 7 showed regression models for predicting the influence of age, sex, BMI and PA on HRQoL. Additionally, the results showed that age, sex, BMI, and PA were significantly predictive of physical functioning (R2=0.24, P<0.001), RLdPhp (R2=0.12, P<0.01), RLdEmp (R2=0.14, P<0.02), general health (R2=0.12, P<0.01), emotional well-being (R2=0.06, P<0.03), PCS (R2=0.18, P<0.001), and MCS (R2=0.15, P<0.01).

Physical activity and body weight status predicting physical functioning, role limitation due to physical health and role limitation due emotional problem of health-related quality of life (multiple regressions of significant predictors, in blocks)
DISCUSSION
This study investigated the joint predictability of PA and BWS on HRQoL of Nigerian patients with mild to moderate hypertension. Finding from our study showed that a majority of participants in this study was either overweight or obese. This is consistent with findings of previous studies that increasing body weight is associated with high prevalence of hypertension (Wang et al., 2006; Wolk et al., 2003). Similarly, evidence from previous studies showed that presence of increased body adiposity especially abdominal fat is an important risk factor for hypertension and CVD event (Doll et al., 2002; Tesfaye et al., 2007). The plausible explanation for this may be due to persistent peripheral resistance, heavy afterload on the heart and damage to the autonomic nervous system, thus, causing increased sympathetic nerve activity, and disrupting the renin-angiotensin systems (Beevers et al., 2001; Giles et al., 2005). This disruption and several obesity-related issues, psychological, psychosocial and adverse effects of antihypertensive medications are likely risk factors associated with impairment of HRQoL of patients with hypertension (Ogunlana et al., 2009; Pan et al., 2011).
Findings from our study show that the HRQoL of participants with sufficient PA is significantly higher (better) than those with insufficient PA. This is similar to findings of previous study that individuals with hypertension who participate regularly in PA programme are more likely to have better HRQoL than their sedentary counterparts (Jeon et al., 2009; Tsai et al., 2004). Exercise has the capability to improve cardiovascular health by increasing cardiorespiratory fitness, lowers blood pressure and increase self-esteem and subsequently improve HRQoL (Mutrie, 2000; Warburton et al., 2006). Furthermore, PA was found to have significant correlation with all subscales of HRQoL. The reason for the significant relationship may be as a result of brain’s contribution to the activation and releasing of endogenous substances including serotonin, beta-endorphin and beta-lipotrophin during regular physical exercise (Meeusen and De Meirleir, 1995; Schwarz and Kindermann, 1989). It is believed that the impact of PA on physiological and psychological functioning bring about a sense of euphoria and pleasure as well as low risk of depression and subsequently lead to improved HRQoL.
On the contrary, there were no significant correlation between PA and each of RLdEmp, emotional well-being and bodily pain domains. This is inconsistent with findings of previous studies which stated that regular PA is capable of relieving emotional well-being and reduce risk of depression (De Moor et al., 2006; Dunn et al., 1999). The possible explanation for nonsignificant relationship may be as a result of other factors affecting overall health of individuals with hypertension. Hypertension is associated with labelling, adverse effect of antihypertensive medications and anxiety and this probably responsible for lower scores in the aforementioned subscales. Similarly, findings from our study show that two subscales of the HRQoL including RLdPhp and RLdEmp had the worst scores. This may be due to common symptoms such as fatigue, frequent headache, dizziness and comorbidities associated with hypertension (Ketelhut et al., 2004; Kjellgren et al., 1998).
Optimal body composition and body weight control is an important lifestyle modification for achieving healthy living (Kohl et al., 2012). Though body weight might not drastically reduce in most individuals participating in PA programme and rehabilitation, appreciable improvement in cardiovascular health and HRQoL appear to be better than individuals who are less active (Maruf et al., 2013; Pan et al., 2011). In our study, when adjusted for body weight, participants with sufficient PA irrespective of body weight status demonstrated better HRQoL than those with insufficient PA despite normal weight. This finding substantiates the fact that sufficient PA is beneficial for healthy living and predicts better HRQoL among individuals with hypertension. The PA level of participants in our study appears to be moderate. This is contrary to findings of previous studies that patients with hypertension usually have low PA level (Awotidebe et al., 2016; Eugene and Bourne, 2013). The moderate PA level observed in our study might be due to regular advice received from physicians and other healthcare professionals emphasizing participation in regular and sufficient PA programme in addition to daily antihypertensive medications. Similarly, in our study, we found that the impact of PA was more pronounced on HRQoL regardless of body weight status. This corroborated findings of previous studies that PA is strongly associated with overall well-being, reduce risk of CVD event and adequate HRQoL (Hallal et al, 2012; Warburton et al., 2006). There is no doubt that persistent physical inactivity and increasing body weight gain in hypertension are important malefactors for unprecedented risk of CVD event and poor HRQoL. Undoubtedly, Warburton et al. (2006) concluded that there is incontrovertible evidence that regular PA contributes to the primary and secondary prevention of several chronic diseases and is associated with a reduced risk of premature death such that most physically active people are at the lowest risk.
The outcome of this study should be interpreted with caution because of some limitations inherent therein. The PA and HRQoL were assessed using the self-reported questionnaire which might be overestimated or underestimated. More importantly, the HRQoL is a variable that can only be subjectively assessed and many factors including individual’s mood, circumstances surrounding treatment such as the provision of adequate medical services, and personal challenges or achievements may influence the assessment of HRQoL. Upto this present moment, there appears to be scarcity of disease specific-HRQoL instrument for patients with hypertension, hence, only generic ones are in use among this population. However, regardless of SF-36 being a generic instrument for assessing HRQoL, several studies have used it among patients with hypertension and found it appropriate in the assessment of HRQoL. For future research involving PA assessment, we suggest that PA assessment should include objective measures such as pedometer-determined PA in order to valid findings of this study. In conclusion, patients with mild to moderate hypertension who reported sufficient PA demonstrated higher and significant HRQoL than those with insufficient PA irrespective of body weight status. Furthermore, sufficient PA is a better predictor of HRQoL among patients with hypertension thus, supporting findings from previous studies. It is important to consider regular assessment of HRQoL of patients with hypertension in order to identify individuals at risk of poor health status and thus provide immediate care in order to achieve both physical and mental well-being. More importantly, regular PA is recommended for patients with hypertension to improve cardiovascular health and satisfying HRQoL.
ACKNOWLEDGEMENTS
The authors wish to thank the Consortium for Advanced Research Training in Africa (CARTA) for providing technical support. CARTA is jointly led by the African Population and Health Research Center and the University of the Witwatersrand and funded by the Wellcome Trust (UK) (Grant No. 087547/Z/08/Z), the Department for International Development (DfID) under the Development Partnerships in Higher Education (DelPHE), the Carnegie Corporation of New York (Grant No. B 8606), the Ford Foundation (Grant No. 1100-0399), Swedish International Development Corporation Agency – SIDA (grant: 54100029), Google.Org (Grant No. 191994), and MacArthur Foundation Grant No. 10-95915-000-INP.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.