Tai Chi Chuan can improve balance and reduce fear of falling in community dwelling older adults: a randomized control trial
Article information
Abstract
Fear of falling and balance impairment are prevalent in older adults and cause major morbidities for this population. The aim of this study was to evaluate the effect of Tai Chi Chuan on balance and fear of falling in community-dwelling older adults. This study was a single-blind randomized control trial. Sixty older adults were randomly allocated into two groups using a 4-cell random block design. The participants of intervention group were trained in Tai Chi Chuan for eight weeks, twice a week, and 55 min in each session. Balance and fear of falling were assessed by Timed Up and Go (TUG) test, Tinetti test and Falls Efficacy Scale International in baseline and after 8 weeks. After eight weeks of intervention, the mean scores of the TUG and Tinetti scales in the intervention group were improved significantly compared to the baseline and the control group (P<0.001). Moreover, the intervention group showed a significant reduction in fear of falling scores (P<0.001), while those in the control group remained unchanged. Tai Chi Chuan effectively improves the balance and fear of falling and could be considered as a practical and useful method for fall prevention in community-dwelling older adults.
INTRODUCTION
Falls are frequent and disabling issues among older adults that influence their health, independence, and quality of life (Hu et al., 2016; Huang et al., 2017; Ku et al., 2013; Li et al., 2005). It has been estimated that 35% to 40% of older adults (age 65 years and older) have at least one fall annually and this incidence rate increases with age (Huang et al., 2017; Li et al., 2005; Tsang and Fu, 2016).
The risk factors for falls can be categorized into two groups: intrinsic factors such as the history of previous falls, age, gender, living alone, other comorbidities, visual impairment, polypharmacy, fear of falling, muscle weakness, gait and balance impairment, and cognitive impairment; and extrinsic factors such as environmental hazards, unsuitable walking aids, and poor footwear or clothing (Du et al., 2017; Logghe et al., 2009). Some of these are modifiable such as balance and gait impairments, muscle weakness, and fear of falling (Cruz-Díaz et al., 2015; Hita-Contreras et al., 2015; Shariat et al., 2018). Fear of falling is an anxiety syndrome in the older adult population that has been defined as an exaggerated concern about falling or the belief that one cannot prevent a fall (Cruz-Díaz et al., 2015; Kumar et al., 2016; Scheffer et al., 2008). The fear of falling has serious consequences in older adults, such as decreased physical and social activities that in turn influences their quality of life. The prevalence of fear of falling has been estimated between 21% and 58% (Cruz-Díaz et al., 2015; Hita-Contreras et al., 2015). The consequences of falls can range from minor problems such as skin abrasions to significant injuries such as hip fractures or head trauma (Zhou et al., 2018).
Since falls among older adults increase health care costs, reducing the incidence of falls is an important public health mission (Okubo et al., 2017). Several preventive strategies have been developed to address the risk factors for falling (Gale et al., 2018; Pengpid and Peltzer, 2018; Zhou et al., 2018). Recently it has been reported that exercise programs, particularly those including balance training, reduces the risk of falls. Tai chi Chuan, which includes a set of strength and balance-training exercises, was found to be effective at preventing falls (Li et al., 2005; Vieira et al., 2016).
Tai Chi Chuan was initially developed as a martial art in China and it has been frequently used as an exercise to improve mental or physical health in young and old populations (Zhao et al., 2017). Tai Chi Chuan consists of a series of dance-like, slow and continuous movements. It emphasizes trunk rotation, weight shifting, coordination and a gradual narrowing of the lower extremity stance (Allen et al., 2011; Wu et al., 2016). Previous studies have shown that Tai Chi Chuan is beneficial for a range of health-related outcomes, including blood flow, neuromuscular function, and cognitive function, as well as decreasing stress reactivity (Rogers et al., 2010).
A few studies have shown that Tai Chi Chuan is effective in preventing falls and improving balance, muscle strength, proprioception, and endurance in older adults (Hu et al., 2016; Lan et al., 2013; Logghe et al., 2010). For example, Gallant et al. (2017) demonstrated that a 12-week Tai Chi Chuan program can significantly reduce the risk of falling in participants. Furthermore, Tai Chi Chuan is comparable to a balance-focused training program in enhancing the lower extremity muscle strength, agility and balance, as well as aerobic endurance in older adults (Yang et al., 2015). However, some studies showed that 12 months of practicing Tai Chi Chuan does not change the fall risk in older adults living at home (Logghe et al., 2009).
Therefore, Tai Chi Chuan remains controversial in literature (Logghe et al., 2009; Yang et al., 2015), thus further studies are needed to elucidate the benefits of the Tai Chi Chuan program in the older adult population. Therefore, we aimed to examine the effects of Tai Chi Chuan on balance and fear of falling in the older adults living at home in a sample from Iran. It is hypothesized that Tai Chi Chuan will improve balance and fear of falling in the older adults.
MATERIALS AND METHODS
Study type
This study was a single-blind randomized control trial (RCT) that followed the CONSORT (consolidated standards for reporting of trials) statement (Fig. 1). This study was registered at the Iranian Registry of Clinical Trials (Registration number: IRCT 2016121931465N1). Ethical approval was obtained from the Faculty of Nursing and Midwifery, Tehran University of Medical Sciences (IR.TUMS.FNM.REC.1395.323).
Participants
All the participants were selected from one single institution. After interviewing older adults in a retirement center in district 6 of Tehran, explaining the goals of the study, and acquiring informed consent, 60 older adults (27 females and 33 males) were randomly assigned to control and intervention groups (Fig. 1).
The inclusion criteria were as follows: Age between 60 and 80 years, ability to walk independently without assistive devices, ability to participate in exercise sessions, and being a member of the Local Retirees Association. The exclusion criteria were as follows: Acute or chronic diseases that interfered with or were exacerbated by exercise, decompensated cardiovascular diseases, neurological diseases affecting mobility (e.g., Parkinson disease, stroke, or multiple sclerosis), significant musculoskeletal diseases (e.g., lower limbs arthroplasty, history of lower limb fractures, and severe deformity in lower limbs or severe osteoarthritis), cognitive disorders (scores below 24 in Mini-Mental Status Examination based on physical examination), and participating in other parallel exercise programs.
Randomization and allocation
We divided the participants into two groups (control and intervention) according to random block and allocated according to computer-generated list of random numbers. None of the participants were aware of the group assignments and randomization procedures. Although the participants and researcher were aware of the group allocation, assessors and data analysts were blinded to the allocation.
Intervention
The Tai Chi Chuan exercise is characterized by balancing the body, mind, breathing, and emotions and making the body’s muscles flexible and empowered (Son et al., 2016). Tai Chi Chuan has 5 major styles (Yang, Chen, Wu, Hao, and Sun) and more than 108 forms. All these styles share similar principles, but each has special features and characteristics. Yang style, as the most common form, has been simplified by Chinese government in the early 21th century to create a 24 unique movements for public use as a form of exercise. This style consists of slow, smooth, and rhythmic movements that put an emphasis on trunk rotation, weight shifting, coordination, and a gradual narrowing of the lower extremity stance (Wu et al., 2016).
In our study, we interviewed people in a local retiree association and explained the goals of the study. Participants who met the inclusion criteria and agreed to participate in the study filled out an informed written consent. In the first session, we assessed the balance and fear of falling in all participants. The participants in the intervention group performed the yang style of Tai Chi Chuan exercise for eight weeks, twice a week, and 55 min per each session. Each session consisted of 5-min warm-up, 35-min Tai Chi Chuan practice, and 5-min cool-down. The entire program was administered by an expert coach of Tai Chi Chuan accompanied by a researcher (LH) in an outdoor location at a community park. The control group did not receive any intervention. At the end of the study, all participants were reassessed for balance and fear of falling. Finally, after the intervention period, the participants of control group were referred to participate in Tai Chi Chuan program.
Intervention fidelity
We assessed the treatment fidelity of study by a standard guideline (Bellg et al., 2004). To ensure the exercise program was administered by the same frequency and duration of sessions for all participants. All trainers and participants expressed some level of enjoyment or satisfaction with the study and none dropped out of the study. To ensure standard training, the entire program was administered and monitored by an expert in Tai Chi Chuan exercises; who is a board member of the Tai Chi Chuan committee in the National Martial Art Federation. To ensure the receipt and enactment of treatment, one of the researchers (LH) controlled the participants’ ability to use cognitive instructions and to perform behavioral skills appropriately.
Measures
The primary outcomes of this study were balance and fear of falls among older adults. Balance was assessed twice at the baseline and at the end of study by Timed Up and Go (TUG) test and Tinetti test. TUG evaluates the mobility function in the older adult population who can walk independently. The participants were asked to wear their usual shoes (they could also use their assistive device), then sit down on a chair. Upon our command to start, they stood up and walked 3 m on straight line, returned on the same path, and finally sat down on the chair. The duration time was measured from the moment that the participant started to stand up from the chair until she/he returned and sat down. Data were classified as follows: Time less than 10 sec (independent mobility), time between 10 and 20 sec (almost independent mobility), times more than 20 and less than 30 sec (mobility is vulnerable), and time ≥30 sec (impaired mobility). The validity and reliability of the TUG have been confirmed in several studies (Akbari et al., 2010; Nordin et al., 2008). Furthermore, our study showed a good content validity and excellent internal consistency (alpha=0.927) for TUG.
Tinetti test was also used for gait and balance assessment in our study. Tinetti test has two parts: Part 1 evaluates balance and consists of nine motor functions; and each item scores 0–1 or 0–2 with a maximum score of 16. Part 2 assesses gait and includes seven types of movement that participants are asked to stand up (with or without assistive device); walk slowly and then walk fast along a predetermined path. Each item scores 0–1 or 0–2 with a maximum score of 12. Total Tinetti scores below 18 predict a high risk of falling; scores between 19 and 23 predict a medium risk of falling, and scores higher than 24 predict a low risk of falling. In line with previous studies, we showed an acceptable validity and reliability (alpha=0.886) of the Tinetti test (Kloos et al., 2004; Tinetti, 1986). In fact, we recruited a healthy population with different levels of balance function, but all were in normal range.
Fear of falling was assessed by the Falls Efficacy Scale International (FES-I). This scale is similar to a likert-type scale and includes 16 questions. The participants were asked to determine the level of their concern about falling while performing 16 different activities on a 4-point likert scale including “I never worry about falling,” “I sometimes worry about falling,” “most of the times I worry about falling,” and “I always worry about falling.” The total score is between 16 and 64; and lower scores indicate less fear of falling. The validity and reliability of FES-I have been previously reported by several studies (Delbaere et al., 2010; Tinetti et al., 1990; Yardley et al., 2005), our further analysis showed a good content validity and an excellent internal consistency (alpha= 0.972). Furthermore, demographic information including age, gender, education, ethnicity, marital status, history of falls during previous year, and number of falls were recorded.
Sample size
Based on previous studies, we calculated the sample size by G×Power from the total available older adults in the retirement center. Total sample size was estimated to be 30, however to reduce the effect of drop out; we decided to recruit 60 participants (Jabarouti et al., 2014).
Statistical analysis
Data management and analysis were performed using IBM SPSS Statistics ver. 21.0 (IBM Co., Armonk, NY, USA). Demographic data were reported by mean, standard deviation, and frequency across both the control and intervention groups. Between group analyses, before and after intervention, were done by independent t-test analysis. Within group differences were analyzed by paired t-test in each group. Independent two sided t-test analyzed difference of mean values of the TUG test and Tinetti test between intervention and the control group. P-value of <0.05 has been considered as significant.
RESULTS
Demographic characteristics and baseline measures
Table 1 shows the demographic characteristics and number of falls the participants in the previous year. There were no significant differences in intervention and the control groups about demographic characteristics.
Balance and fear of falling between the two groups before intervention
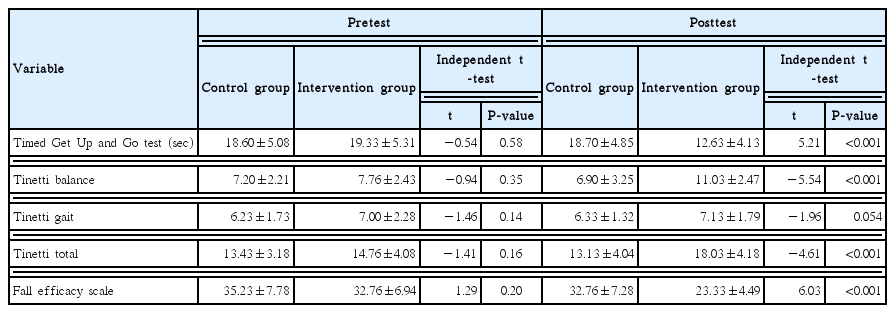
Table 2 shows the baseline values for TUG, Tinetti test, and FES-I in the control and intervention groups. In the two groups, there was no statistical difference in the gait and balance mean scores (TUG and Tinetti) at the baseline (P>0.05). Between- group analysis showed that there was also no difference in the FES-1 mean at the baseline (P>0.05).
Balance and fear of falling between the two groups after intervention
As Table 2 shows, between-group analyses indicated that there was a statistical difference in the balance and fear of falling scores after intervention (P<0.001). In fact, the intervention group showed a better balance and less fear of falling compared with the control group. However, there was no difference in Tinetti (gait section) between the two groups after intervention (P>0.05).
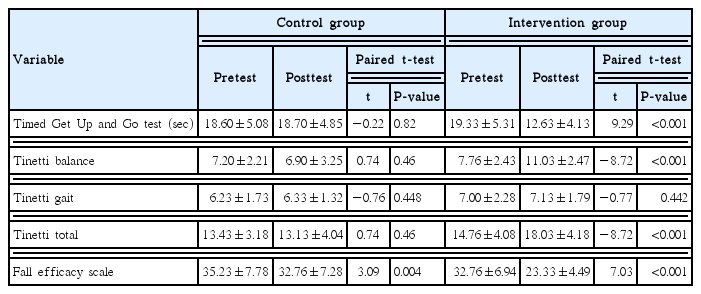
Balance and fear of falling within groups
Table 3 shows TUG, Tinetti, and FES-I scores in the intervention and control groups. In the control group, analyses revealed no significant difference in TUG, Tinetti, and FES-1 comparing pre-test and post-test values. While in the intervention group, participants showed a significant improvement in TUG, Tinetti (balance and total scores), and FES-1 after intervention period. Only Tinetti scores of gait section did not differ between pre-test and post-test in intervention group.
DISCUSSION
Our study confirms the hypothesis that Tai Chi Chuan exercise improves the balance and fear of falling in community-dwelling older adults. This finding is in agreement with several previous studies that showed that Tai Chi Chuan improves the balance in the older adults (Ćwiękała-Lewis et al., 2017; Hu et al., 2016; Yang et al., 2015). For instance, Yang et al. (2015) found that Tai Chi Chuan had positive effects on the balance, gait, and quality of life in older adults with Parkinson disease after 8 weeks. Several factors contribute to impaired balance during the aging process, including a reduction in fast twitch fibers, nerve conduction velocity, muscle flexibility, and development of osteoarthritis that indicate a need for intervention (Zhang et al., 2006). It is expected that Tai Chi Chuan movements could improve the balance in the older adults by shifting the center of gravity, weight shifting between legs, heel to toe and multidirectional stepping (Wu et al., 2016). There are some studies that showed no benefit in improving the balance and risk of falls after 13 weeks in older adults. It could be due to the characteristics of the study population who had good balance function at the baseline (Logghe et al., 2009). In other words, Tai Chi Chuan may be more effective in the older adults with balance problems and prevent falls in the high-risk older adults.
In the current study in line with existing literature, we also found that Tai Chi Chuan significantly reduces the fear of falling score. For example, Sattin et al. (2005) demonstrated that Tai Chi Chuan compared to wellness education programs such as diet and nutrition program; pharmacological management; legal issues relevant to health; changes in body function; and mental health issues, such as stress, depression, and life changes improves fear of falling in frail adults aged 70–79 years. However, some prior studies could not show sufficient evidence about the effect of Tai Chi Chuan on fear of falling in the older adults (Logghe et al., 2009; Logghe et al., 2010). The difference could be due to the heterogeneity of samples; for example, in one of the studies, the participants had a low fear of falling at the baseline, thus no large improvement in fear of falling was found in study’s population after intervention period. There is an inverse relation between the fear of falling and physical activity in the older adults; so that a decrease in physical activity can also result in a higher rate of falls and vice versa (Jeon et al., 2014; Legters, 2002). In fact, the slow movements of Tai Chi Chuan increase the level of concentration and attention, which helps a person to maintain calm and relaxed in critical and stressful situations. In other words, when a person performs Tai Chi Chuan movements in a calm place with deep and slow breathing, s/he will experience a sensation of physical and psychological relaxation and well-being (Miller and Taylor-Piliae, 2014; Zhao et al., 2017).
Our study showed that Tai Chi Chuan significantly improves the balance and fear of falling in community-dwelling older adults. On the other words, Tai Chi Chuan is a valuable exercise for the older adults, especially those with lower balance skills and at risk of falling.
Since falling has a physical, psychological, and economic burden for older adults, they need a simple and economical intervention that does not require special equipment and they can simply do it. Tai Chi Chuan exercises is one of the simple and economical interventions that can be used as a preventive intervention and taught in geriatrics clinics to the older adults at risk of falling. However, it is advisable to perform further studies to examine the generalizability of our findings across different subjects and social settings. Furthermore, it could be interesting to evaluate the effect of Tai Chi Chuan on biological and physiological markers in the older adults.
Totally this study had several limitations; for example, the study did not conduct follow ups to evaluate the risk of falling once the intervention ceased to report any long-lasting impact. Since the participants and researchers were not blind to their group allocation the generalizability of the findings were limited. The participants were limited to older adults who lived in one conditions including cultural environment, economic situation, and social settings of their residence.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
ACKNOWLEDGMENTS
The authors would like to express their gratitude to all patients and instructors who participated in the study.