Effect of combined aquatic and cognitive training on quality of life, fall self-efficacy, and motor performance in aged with varying cognitive status: a proof-of-concept study
Article information
Abstract
With the increasing number of aged individuals, research pertaining to their cognitive functions and physical-motor has become exponentially imperative. The purpose of the study was to investigate the effect com-bined aquatic and cognitive training on quality of life (QoL), fall self-effi-cacy and motor performance (static and dynamic balance) in aged with varying cognitive status levels. Thirty participants were assigned to a high cognitive status group (n=10), low cognitive status group (n=10), or nonintervention control group (n=10). Participants completed a 6-week motor-cognitive training regime with increasing intensity. QoL, fall self-efficacy, static balance, and dynamic balance were assessed. Preliminary results suggest proof-of-concept significant (P<0.05) im-provements were found in both the high and low cognitive status groups for static and dynamic balance and fall self-efficacy. However, QoL was only found to be significantly improved in the low cognitive status group. Aqua training along with cognitive training can effectively be used to prevent falls in the elderly and to improve their physical-motor perfor-mance. However, when attempting to improve QoL, the cognitive status of the individual should be considered.
INTRODUCTION
Aging is a process that occurs over time and leads to deleterious structural and functional deviations in the body. Physical and cognitive impairment represent two of the most acute of these changes among the elderly because they can lead to physical dependence and social isolation (Lee et al., 2019). According to the United Nations statistical estimates, about 2.5% of the population over the age of 65 is added annually, and by 2025 one out of every seven people in the world is expected to be over 60 years old (Mangine et al., 2014). Iran is no exception to this phenomenon and according to the latest population and housing census of 2016, the population of people over 60 years is over 7,400,000 people, which makes up about 10% of the total population (Fuladvandi et al., 2017). Life expectancy in Iran has been reported to be 73 years (Delavari et al., 2016).
One-third of the elderly have cognitive disabilities, and more than 60% of them need help with daily activities. Taken together, the interconnected nature of physical and cognitive function emphasizes the importance of cognition when examining physical function in the elderly (Aliberti et al., 2019). Specifically, dysfunction in executive functions (such as working memory, inhibition, transitive attention) and psycho-verbal in the elderly are accompanied by many declining changes in health and physical function and is manifested by an increased risk of falls (Goudarzian et al., 2017; Schoene et al., 2015). Falling is the third leading cause of chronic disability in the world (Desjardins-Crépeau et al., 2016). In fact, the incidence of falls in the elderly with cognitive deficits is approximately 60% higher than in individuals with normal cognitive status.
Cognitive problems in the elderly include memory loss and difficulties in recognizing time, place, etc. (Petersen et al., 2014). It develops with varying severity and, depending on the severity, leads to behavioral disturbances in the elderly and may have other negative social consequences (Lachs et al., 1992).
In the field of exercise science, practitioners are always searching for nonpharmacological This is because exercise has been shown to affect both the psychological and physiological factors that are associated with decreased quality of life due to aging (Sanders et al., 2019; T O’Dwyer et al., 2007). However, while exercise is seen as a promising intervention to prevent or delay cognitive decline in individuals aged 50 years and older, the evidence is not conclusive (Northey et al., 2018). In addition, while some clinical trials of exercise interventions demonstrate positive effects of exercise on cognitive performance, other trials show minimal to no effect (Kirk-Sanchez and McGough, 2014). This may be so since exercise programs may need to be structured, individualized (to cognitive status) and be multicomponent in design to show promise for preserving cognitive and physical performance in older adults (Kirk-Sanchez and McGough, 2014). Problematically, while studies investigating the impact of aquatic exercise on cognition are scarce (Ayán et al., 2017), and no studies have been performed on a subgroup analysis of the effects of exercise interventions on different cognitive domains of the elderly (Zhou et al., 2018). In addition, since water-based exercise provides the same physiological benefits as land-based exercise with reduced risk of acute injury (Fedor et al., 2015), especially from falls, the present study novely attempted to determine if a multimodal therapy of aquatic exercise and cognitive training could improve on motor performance and quality of life in aged. Further, the present study uniquely attempted to determine if this multimodal therapy is more effective on those with low or high cognitive status in order to individualize and target program design.
MATERIALS AND METHODS
Study design
This study made use of a quasi-experimental proof-of-concept design for this potential application of combining aquatic and cognitive training to improve motor performance and quality of life in the aged with varying cognitive status. The study protocol was approved by University of Tehran, Iran (ID: IR.SSRI.REC. 1398.624). In order to determine feasibility via proof-of-concept, but not represent deliverables of subgroup analysis of the effects of exercise interventions on different cognitive domains of the elderly (Zhou et al., 2018), 30 previously sedentary participants aged 60 years and above (Northey et al., 2018; Resende-Neto et al., 2019) were randomly assigned to a low cognitive status group (n=10), high cognitive status group (n=10), or a control group (n=10), whose participants continued with their normal daily activities. Participants were community-dwelling female volunteers (aged from 60 to 70 years; average, 63.57±3.31 years). Interested individuals were screened to determine whether they met the inclusion and exclusion criteria. For inclusion, participants had to be older than 60 years, have a fluency of Persian; had to sign the informed consent; were required have the ability to respond to questionnaires, including the Mini-Mental Status Questionnaire (MMSE); have no absolute or relative contraindications to exercise and be willing to use the intervention for six weeks (Ansari et al., 2010; Shariat et al., 2018). Exclusion criteria included seniors with diagnosed Alzheimer disease, dementia, recent head injury, or unstable chronic diseases (e.g., stroke, diabetes), rapidly progressing or terminal illnesses (Eggenberger et al., 2015), or a score not being classified as having a low or high cognitive status on the MMSE.
Measurements (primary outcomes)
An MMSE was used to assess cognitive status (MacKenzie et al., 1996) with the validity of the Persian version of this questionnaire being developed previously (Ansari et al., 2010). The World Health Organization quality of life questionnaire was used to measure quality of life. The questionnaire consisted of 26 questions in four domains: physical health, psychological, social relationships and environmental (Juniper et al., 1994). The international fall depression self-esteem inventory questionnaire was used to collect falling self-efficacy data. Static balance was evaluated by the adjusted Romberg test (McIlroy and Maki, 1997). Dynamic balance was measured using the Timed Up & Go test in which the participants were required to rise from the chair, walk three meters, turn around, walk back to the chair and sit down (Hakakzadeh et al., 2019).
Interventions
After the pretest measurements, the participants in the intervention protocols followed an exercise regime based on that of Jung et al. (2014) and Means and O’Sullivan (2000) for 6 weeks, 3 times weekly (Jung et al., 2014; Means and O Sullivan, 2000). The pool was 7×6 m and 110 cm in depth. The water temperature was kept at 30°C–33°C for the aquatic exercises. Each session commenced with a 15-min warm-up, followed by 40 min of aquatic training and concluding with a 5-min cool-down. The water-based program consisted of incremental bodily exercises.
In order to implement obstacles and stepping-stones in water, the IGYM system (ISOPA, Hwasung, Korea) was used together with the pool step. After installing the round towers, they were connected by bars at the height of the holes to make an obstacle. The obstacle training consisted of three subparts, stepping over the IGYM system, going up and down stairs, and crossing over a step. The obstacle training was as follows. Warm-up included upper extremity and lower extremity stretching and range of motion exercises for flexibility (15 min). The main exercise included stepping over the IGYM (a height of 10 cm), stepping over the IGYM (a height of 20 cm), going up and down stairs (a height of 19 cm), crossing over a step (a height of 14 cm), and turning around a target and returning along the obstacle course for 20 min. Participants combined these exercises with other tasks intended to stimulate cognitive functions through movement using BrainGym therapy for an additional 20 min (Dennison and Dennison, 1989; Morgenstern et al., 2017). At first only simple motor tasks were performed, then gradually simple cognitive tasks were added to the motor tasks; in turn, both motor and cognitive tasks became more complex. Cool down included upper extremity and lower extremity stretching and range of motion exercises for flexibility (5 min) (Jung et al., 2014; Means and O Sullivan, 2000). All sessions were supervised by the primary investigator. The control group was not assigned any intervention and was required to continue with their normal daily activities.
Statistical analyses
After the posttest, the data were monitored and normalized. A Shapiro–Wilk test using tilting and elongation indices were applied, and the data normality was determined based on Q-Q graphs. Then by analysis of compound variance test 2×3 (2 groups: high and low cognitive status and 2-step control measures: pretest, posttest) with repeated measurements on the latter factor, the data were analyzed, and in terms of discriminant analysis of within-group effects, a paired t-test was used.
RESULTS
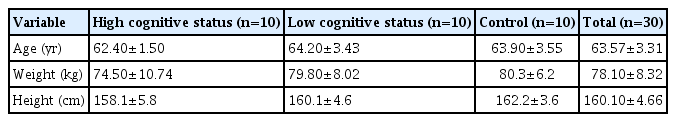
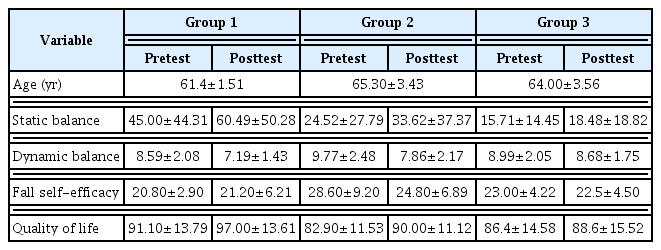
Demographic characteristics of the participants are shown in Table 1. Statistical analysis showed that the three groups were homogenous (P≤0.05) for age, quality of life and fall self-efficacy, they were heterogeneous for static and dynamic balance (Table 2). The results obtained following the 6-week intervention indicated that significant improvements were found in both the high and low cognitive status groups for fall self-efficacy, static and dynamic balance. However, quality of life was only found to be significantly improved in the low cognitive status group.
The results of the compound variance analysis test that was performed to investigate the effects of the intervention and intergroup effects after assuring homogeneity of covariance with the result of the Box M test are presented in Table 3. Findings show that all variables have a significant main effect of time, i.e., interventions lead to a meaningful effect on dependent variables (P≤0.05). It was found that static and dynamic balance and self-efficacy, main effect, and interactive effect were not significant, whereas, quality of life, the main effect and the interactive effect were significant. As such, the changes in the high and low cognitive status groups were the same for quality of life, static balance and dynamic balance. However, a significant difference was found between the high and low cognitive status groups for self-efficacy.
DISCUSSION
The purpose of the study was to investigate the effect combined aquatic and cognitive training on quality of life, fall self-efficacy and motor performance (static and dynamic balance) in aged with varying cognitive status levels. Despite the three groups were homogenous for age, quality of life and fall self-efficacy, they were heterogeneous for static and dynamic balance. This is to be expected since cognitive problems in the elderly lead to behavioral disturbances in the elderly and may have other negative social consequences, such as an increased sedentary behavior (Lachs et al., 1992; Petersen et al., 2014). Problematically, the findings of this study are unique in that studies investigating the impact of aquatic exercise on cognition are scarce (Ayán et al., 2017), and no studies have been performed on a subgroup analysis of the effects of exercise interventions on different cognitive domains of the elderly (Zhou et al., 2018).
While aquatic exercise has been demonstrated to improve cognitive function in the elderly (Ayán et al., 2017; Sato et al., 2015), the findings of the present study demonstrated inconsistent results that combined aquatic and cognitive training only improved quality of life in elderly individuals with a low cognitive status. While further research is needed to confirm or disprove this unique finding, these findings may again highlight the importance of personalized prescription for water-based exercises in elderly adults to improve cognitive function. The finding that both the low and high cognitive status groups improved their fall self-efficacy is an important finding. This is because fear of falling is an important barrier to many activities, including participation in structured exercise programs since it is with distress, increased use of medication, decreased physical function, increased risk of falls, reduced quality of life, activity restrictions, fractures, and admission to institutional care (Dewan and MacDermid, 2014). It must also be noted that the use of water-based exercises in the aged is especially important to not only reduce falling but also to mitigate the distress associated with a low fall self-efficacy.
Balance is an important part of the functional evaluation in older adults when screening for falls (Cuevas-Trisan, 2017). While land-based exercise is generally regarded to improve balance, and specifically dynamic balance, more than water-based exercise in several populations (Eyvaz et al., 2018; Silva et al., 2008), it must again be noted that the use of water-based exercises in the aged is not only important for those elderly with osteoarthritis, but also to reduce actual falling, and to allay the distress associated with a fear of falling. While previous water-based studies have demonstrated improvements in static balance (Jung et al., 2014), the present study’s unique finding that the 6-week water-based intervention improved both static and dynamic balance in both the high and low cognitive status groups is particularly noteworthy. This may be related to not only improvements in motor control, but also in improved cognitive function associated with cognitive training as utilized in the present study (van Het Reve and de Bruin, 2014). The finding that exercise can improve balance in elderly groups with high and low cognitive status has previously been demonstrated, albeit following land-based strength-balance- cognitive training (van Het Reve and de Bruin, 2014).
The present study has several limitations that could affect ecological validity. In this regard, the small sample size, while similar to that of numerous previous studies (Fedor et al., 2015; Jung et al., 2014; Means and O Sullivan, 2000; Sato et al., 2015) serves as proof-of-concept evidence for the effect of the effect combined aquatic and cognitive training on quality of life, fall self-efficacy and motor performance (static and dynamic balance) in aged with varying cognitive status levels. In addition, several extraneous variables could affect quality of life, fall self-efficacy and motor performance (static and dynamic balance). In this regard, alterations in various factors that were not measured in the present study, such as socioeconomic status, income, marital status, could have affected quality of life (Zhang et al., 2019).
Aquatic exercise is a safe and effective intervention in the elderly with cognitive deficits and/or at risk of falling. Based on the findings of the present study, it seems that by combining aquatic and cognitive training, a new pathway could be utilized to improve the elderly’s quality of life and physical abilities (i.e., static and dynamic balance) to prevent falls. This study also revealed the necessity of considering an elderly individual’s cognitive status prior to prescribing exercise in order to optimize the benefits of exercise.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.