A novel manual therapy technique is effective for short-term increases in tibial internal rotation range of motion
Article information
Abstract
The coupled motions of tibial internal rotation (T-IR) and ankle dorsiflexion (DF) are necessary for proper lower-limb function. Anecdotally, clinicians have been performing techniques to restore T-IR to improve ankle DF, however, no evidence exists to support their efficacy. Therefore, the two objectives were to: (a) determine the effectiveness of a manual therapy technique for improving T-IR range of motion (ROM) and (b) Examine the relationship between ankle DF and T-IR ROM. Twenty-four participants qualified to participate and were randomly allocated to either the control (n=12) or manual therapy (n=12) group. Closed-chain ankle DF and T-IR ROM were assessed at baseline and immediately posttreatment. Control group participants sat quietly for 5 minutes. The experimental group performed 3 sets of 15 repetitions of a manual therapy, mobilization with movement technique. With the patient in a kneeling lunge position, the examiner wrapped an elastic band around the tibia and fibula and was instructed to lunge forward while the examiner simultaneously manually internally rotated the lower leg. T-IR ROM significantly increased following the intervention for the manual therapy group when compared to the control group. There were no significant changes in standing or kneeling DF ROM. No significant correlation was found between T-IR and both standing and kneeling DF ROM. A single mobilization with movement treatment is effective for improving tibial IR ROM in the short-term compared to no treatment. However, active tibial IR and end-range dorsiflexion range of motion do not appear to be correlated based on these methods.
INTRODUCTION
Clinicians routinely quantify and track joint range of motion (ROM) as part of the evaluation and rehabilitation process. Limitations in tibial ROM are often overlooked due to the difficulty in measuring transverse plane motion (Makowski et al., 2005). The embedded compass app of an iPhone (iPhone 6 model A1549, Apple, Inc., Cupertino, CA, USA) has recently been shown to reliably assess tibial internal and external rotation ROM making it convenient and easy to quantify (Stanek et al., 2020). Rotational motion at the tibia is essential for knee and ankle function and is often implicated as a compensatory strategy for various lower extremity conditions (Bell-Jenje et al., 2015; Bonci, 1999; Griffin et al., 2000; Matsumoto et al., 2000; Zhang et al., 1993). Previous authors have described tibial rotation as an important, yet often understudied (Makowski et al., 2005; Matsumoto et al., 2000; Zhang et al., 1993). A thorough understanding of rotational motion of the tibia contributes to an accurate evaluation of knee mobility, as well as provides a better understanding of function at the hip, ankle, and foot.
A previous investigation described potential complications from abnormal variations in tibial rotation (Lusin and Gajdosik, 1983). These pathologies include the development of chondromalacia patella and other degenerative joint changes. Alterations in tibial rotation have also been implicated with meniscal lesions and injuries to the cruciate ligaments (Hallen and Lindahl, 1966). Furthermore, tibial external rotation, along with anterior translation of the knee, and hindfoot eversion have been implicated with dynamic valgus at the knee (Bell et al., 2008; Hewett et al., 2006). This positioning has been correlated with iliotibial band syndrome (Ferber et al., 2010), patellofemoral pain syndrome (Levinger et al., 2006; Molgaard et al., 2011), tibial stress fractures (Milner et al., 2006), posterior tibial tendon dysfunction (Ness et al., 2008), anterior cruciate ligament tears (Powers, 2010), and osteoarthritis of the knee (Chang et al., 2005).
Much of the previous literature has focused on the relationship between hip and knee alignment, especially as it relates to dynamic valgus. However, a more recent study found individuals with <17° of ankle dorsiflexion (DF) exhibited 6.5° higher hip adduction angles during an elevated step down task (Bell-Jenje et al., 2015). Interestingly, the higher hip adduction angles were normalized to the group with >17° DF with a heel lift, suggesting that lost DF ROM contributed to the valgus knee positioning. During normal lower extremity biomechanics, several motions must couple in order to achieve optimal function. For example, during closed-chain activities, the tibia must internally rotate (IR) to allow ankle DF and pronation to occur (McClay and Manal, 1997). Loss of DF ROM is commonly observed in both the athletic and general population and is believed to be a predisposing factor for lower extremity injury (Backman and Danielson, 2011; Neely, 1998; Tabrizi et al., 2000; Wang et al., 2006; Willems et al., 2005; You et al., 2009). Typically, DF ROM deficits are believed to be caused by tightness of the triceps surae, a decrease in the posterior glide of the talus, and/or accessory motion loss at the tibiofibular, subtalar, and/or midtarsal joints (Denegar and Hertel, 2002; Leanderson et al., 1993). Because the motions of DF and T-IR are coupled, lost T-IR could also contribute to deficits in DF ROM. Despite wide ranges in reported normative values for T-IR (Lusin and Gajdosik, 1983; Makowski et al., 2005; Stanek et al., 2020), findings from a previous study using the compass app showed average T-IR ROM to range from 12°–14° (Stanek et al., 2020). Anecdotally, clinicians have been performing techniques to restore T-IR and potentially improve ankle DF. Several variations of the technique using elastic bands have been published in blog or online video posts (Physical Therapy Nation, YouTube, San Bruno, CA, USA) to provide guidance for how to perform the technique, however, no peer-reviewed, published literature exists to support their efficacy. Furthermore, the use of elastic bands, such as the VooDoo floss band (Rogue Fitness, Columbus, OH, USA), is scarce amongst the literature (Kiefer et al., 2017). Therefore, the purposes of this exploratory study were to determine the effectiveness of a manual therapy, mobilization with movement (MWM) technique for improving T-IR and secondarily to examine the relationship between T-IR and DF ROM. We hypothesized that the manual therapy technique would immediately improve T-IR ROM. We also hypothesized that T-IR and DF ROM would be positively correlated.
MATERIALS AND METHODS
Design
An examiner-blinded, cohort study design with randomization was used to examine the impact of the manual therapy intervention on DF ROM. Participants were required to report to the athletic training clinic for a single session. Participants were randomized into to either the control or manual therapy group using block randomization. Limb dominance was self-reported by the participant as the preferred kicking limb.
Participants
Based on a data from a previous reliability study (Stanek et al., 2020), and a simple, online sample size calculator using an alpha level of 0.05 and an intraclass correlation coefficient of 0.85, an estimated sample size of 11 participants per group was recommended. Twenty-seven participants were initially recruited and screened for inclusion. A total of 24 participants (age, 20.1±1.2 years; weight, 68.9±13.5 kg; height, 171.3±10.4 cm) met the inclusion criteria and qualified for the study (Table 1). Participants were recruited via verbal announcements and advertisements throughout the School of Kinesiology and Recreation. All participants were recreationally physically active and needed to meet the inclusion criteria. To be included in the study, participants needed to have less than 12° of T-IR, have no prior history of lower extremity surgery to the limb, and have no recent history (within the past 6 months) of lower extremity injury to the limb. The threshold of 12° was based on a previous study showing average normative values for T-IR ROM measured using a compass app ranged from 12°–14° (Stanek et al., 2020). In total, 42 limbs were randomly allocated to either the control (12 participants) or intervention (12 participants) group. In instances when both limbs of the participant qualified, both limbs were allocated to the same group. Prior to beginning data collection, the Institutional Review Board of Illinois State University reviewed and approved the study (IRB No. 2018-93). All participants provided written informed consent prior to study participation.
Instrumentation
Participants’ T-IR and closed-chain ankle DF in standing and kneeling were assessed immediately before and after the intervention. To assess T-IR, the compass app on an iPhone (iPhone 6 model A1549, Apple, Inc., Cupertino, CA, USA) was secured to the lower leg using the Premium Tribe Sports Armband (Tribe Fitness, Seattle, WA, USA) following previously used methods (Stanek et al., 2020). The smartphone was secured to the lower leg so the bottom of the device rested immediately superior to the ankle mortise.
Closed-chain ankle DF was assessed in both standing and kneeling with a digital inclinometer (SmartTool, Pro 3600, MD Building Products, Oklahoma, OK, USA) on the anterior aspect of the tibia, immediately below the tibial tuberosity. Previous authors have shown this to be a highly reliable method for evaluating DF ROM (Powden et al., 2015; Stanek et al., 2018).
Procedures
All procedures for evaluating T-IR followed the methods of Stanek et al. (2020) for measuring tibial rotation using a smartphone compass app and these methods showed excellent reliability. Based on this study, standard error of the measurement (SEM) for these procedures was 2.24–2.82 (Stanek et al., 2020). Participants arrived at the lab and reviewed the study purpose and procedures by reading through the informed consent document. Participants agreeing to participate signed the informed consent document and completed the preparticipation questionnaire. To standardize activity levels, all participants were instructed to ride a stationary bike with moderate resistance for 5 minutes. Participants removed shoes and socks and sat on an adjustable stool with the height adjusted so the hip and knee angles were at 90°. The phone was secured to the lower leg with the armband so it sat immediately superior to the talocrural joint. Using a vertical plumb line, the test limb was placed in neutral by aligning the tibial tuberosity with the center of the talocural joint. The rater stabilized the participant’s femur and taught the motions of T-IR. As the participant was taught the movement, the individual was asked to maintain the neutral, resting position of the foot in order to avoid excessive pronation and supination. The rater visually verified the movements and the test limb was returned to neutral after each movement. To assess tibial rotation ROM, the rater recorded an initial reading from the compass app while in neutral, followed by the participant moving into T-IR (Fig. 1). The rater recorded a second reading from the compass app at the end ROM, with the difference between the two positions recorded for the measurement. The average of the 3 trials for T-IR was used for analysis.
Next, the participant’s closed-chain DF was measured in standing (Fig. 2) and kneeling (Fig. 3) using a modified weight-bearing lunge test. Previous authors have shown this to be a highly reliable method for evaluating DF ROM (Bennell et al., 1998; Hall and Docherty, 2017; Powden et al., 2015; Stanek and Pieczynski, 2020). The participant stood, positioned the test leg behind the nontest leg on a strip of tape that was perpendicular to the wall, and leaned forward until the first point of stretch was felt in the calf and/or when the heel began to rise. The trial was deemed successful if the test knee remained straight and the heel-maintained contact with the floor. The digital inclinometer was placed on the anterior tibia, immediately below the tibial tuberosity. Next, participants’ kneeling DF ROM was assessed by instructing the participant to kneel on the opposite leg being tested with the test limb visually placed in 90° of hip and knee flexion. The participant placed their front foot on the tape line as previously stated. The participant was then instructed to lunge forward while keeping their heel in contact with the ground and their foot in line with the tape. The participant was instructed to lunge forward until their first felt a stretch in their distal calf and/or the heel began to rise. The inclinometer was placed in the same position as the standing measurement. The average of three measurements was recorded.
Participants allocated to the control group were instructed to sit quietly on the exam table for 5 minutes. Experimental group participants positioned the test limb forward in a kneeling lunge. A 7-foot (2.13 m) VooDoo Floss Band (Rogue Fitness, Columbus, OH, USA) was wrapped with moderate tension from just above the ankle mortise, in the direction of IR superiorly around the lower limb. Next, the participant was instructed to lunge forward while simultaneously the clinician guided the participant into the DF position and internally rotated the tibia. Both the T-IR and DF ROM were moved to end-range with each repetition and each trial was completed to the beat of a metronome set at 45 beats per minute. A total of 3 sets of 15 repetitions of the manual therapy MWM technique were completed with 1-minute rest between sets. These methods followed a modified version of a previously used MWM technique (Collins et al., 2004). All participants had postmeasurements completed using the previously described methods.
Statistical analysis
All statistical analyses were performed using IBM SPSS Statistics ver. 24.0 (IBM Co., Armonk, NY, USA). Preliminary analyses were conducted and showed no difference between groups at baseline for demographics (age, height, and mass), T-IR, standing, or kneeling DF ROM measures (P>0.05). To compare the effectiveness of the manual therapy intervention, change scores were calculated for T-IR, standing, and kneeling DF ROM by subtracting the postmeasurement from the premeasurement. Independent samples t-test were used to determine significant differences between groups. To determine relationships between T-IR and DF ROM, Pearson product-moment correlation coefficient were calculated. Prior to running the analyses, preliminary assumption testing for normality and homogeneity of variance were completed with no violations. Effect sizes were calculated using the Cohen d and categorized as trivial (≤0.20), small (0.21–0.49), moderate (0.50–0.79), or large (≥0.80) (Lakens, 2013). The α level was set a priori at P<0.05.
RESULTS
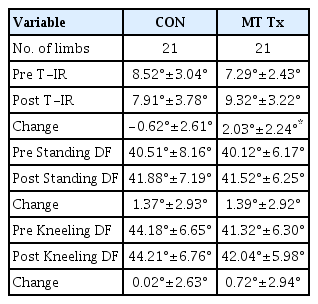
Descriptive statistics for all data are included in Table 2. There was a statistically significant amount of T-IR increase following the intervention for the manual therapy group (m=2.03°±2.24°) when compared to the control group (m=0.62°±2.61°); t(40)= 3.53, P=0.001, effect size=1.09, 95% confidence interval=0.44–1.74. There were no significant changes in standing (t[40]=0.04, P=0.97) or kneeling (t[40]=0.81, P=0.42) DF ROM. No significant correlation was found between T-IR and both standing (r=0.20, P=0.20) and kneeling (r=0.14, P=0.39) DF ROM (Figs. 4, 5).
DISCUSSION
The purpose of this study was to investigate the effectiveness of a manual therapy technique aimed at improving T-IR ROM and examine the relationship between T-IR and DF ROM. Our hypotheses were only partially supported. Results showed a single session of manual therapy can increase T-IR ROM but it had no effect on DF ROM. Additionally, end-range T-IR and DF ROM do not appear to be associated as there were small, nonsignificant correlations between T-IR and both standing and kneeling DF ROM. Because of the test position for the manual therapy technique, we chose to assess both standing and kneeling DF in the event the intervention had a different impact on these measures. However, results showed neither standing nor kneeling DF ROM was impacted from the intervention.
Manual therapy interventions are commonly used within rehabilitation settings, often with the goal of improving mobility. The manual therapy MWM technique employed in this study has been demonstrated online as a method for improving T-IR. Due to the nature of the technique, it is not surprising that it can increase motion since the technique passively moves the tibia into IR with each repetition. However, the weightbearing technique also passively moves the ankle into DF, therefore it was surprising to see no changes in DF mobility. It is possible the participants in this study had adequate DF mobility, creating a ceiling effect for further increases in DF ROM. A study among people with restricted DF mobility may have shown different results.
Reduced ankle DF ROM is a commonly found deficit within athletic and non-athletic populations and is commonly observed in patients following a lateral ankle sprain (Denegar et al., 2002; Hertel, 2002; Hubbard and Hertel, 2006; Tabrizi et al., 2000). However, reduced DF is also a risk factor for sustaining a lateral ankle sprain, therefore, numerous interventions for improving DF ROM have been studied (Terada et al., 2013). Traditionally, treatments for DF ROM deficits include the use of joint mobilizations for restoring the proper accessory motion, stretching of the triceps surae, modalities, or a combination of these therapies (Young et al., 2013). To our knowledge, no previous studies have examined the impact of T-IR ROM on DF mobility. Because previous studies have demonstrated the coupled motions of knee flexion, T-IR, and ankle DF ROM during functional tasks such as squatting or during gait (Bell-Jenje et al., 2015; McClay and Manal, 1997), we hypothesized that improving T-IR may also positively affect DF ROM. However, while the manual therapy intervention was effective at improving T-IR rotation in the short-term, it does not appear that this resulted in an increase in DF ROM.
Tibial IR ROM is not commonly quantified in the clinical environment, yet rotational motion at the tibia is essential for knee and ankle function and is often implicated as a compensatory strategy for various lower extremity conditions (Bell-Jenje et al., 2015; Bonci, 1999; Griffin et al., 2000; Matsumoto et al., 2000; Zhang et al., 1993). A previous reliability study using the same measurement technique showed average T-IR ROM to be approximately 13° with SEM ranging from 2.24–2.82 (Stanek et al., 2020). Because of the large standard deviations in the reliability study, the SEM was high. Using data from the current study and using the formula SEM=standard deviation x-√1-r, with r as the reliability of the measurement, the calculated SEM was 1.46. Collectively, participants in the current study started with approximately 8° of T-IR and participants in the intervention group reached values around 9.3°. Participants in the intervention group demonstrated over a 2° change in ROM with large effect sizes. These findings suggest clinically meaningful changes in T-IR ROM, however, additional research to support these findings is needed. Methods and instrumentation for assessing T-IR ROM vary greatly throughout the literature. Therefore, it is important for clinicians to have the ability to quantify and address limitations when necessary. Our results suggest this technique could be a simple, yet effective method for increasing T-IR in the short term.
This study is not without limitations. First, we measured active, end-range T-IR and DF ROM. While previous authors have demonstrated these motions are coupled during functional tasks, it is possible T-IR occurs early within the functional task and maximum IR occurs prior to end-range DF ROM. Therefore, increasing the T-IR did not have a substantial effect on end-range DF ROM. Secondly, we used a healthy population with limited T-IR ROM, but normative values of T-IR vary considerably. Previously forthcoming work using similar methodology showed T-IR values between 12°–14° (Stanek et al., 2020). Our inclusion criteria required participants to have less than 12° of T-IR to potentially prevent a ceiling effect with the manual therapy MWM technique. Because of the wide variability within previously published normative values for T-IR (Lusin and Gajdosik, 1983; Makowski et al., 2005), less than 12° may not be a sufficiently restricted degree of mobility for T-IR. Furthermore, our population did not have a DF ROM deficit. It is possible our results for changes in DF ROM would have been different if we recruited a population with a known T-IR and DF deficit. Future research is needed to quantify consistent and accurate values for normal tibial rotation mobility. Furthermore, additional research should examine the effects of this manual therapy technique on functional tasks such as gait or squatting. Lastly, we compared a single treatment to a true control condition receiving no intervention. It is possible comparing to another intervention or a placebo intervention could have resulted in different findings.
In conclusion, a single manual therapy, MWM treatment is effective at increasing T-IR ROM in the short-term compared to no treatment. However, it did not affect closed-chain DF ROM. Clinicians are encouraged to examine tibial rotation mobility within their patients for potential deficits. Patients with deficits in T-IR mobility may benefit from using this manual therapy technique.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
ACKNOWLEDGMENTS
The authors received no financial support for this article.