Influence of motor impairment on exercise capacity and quality of life in patients with Parkinson disease
Article information
Abstract
This study evaluated the impact of motor impairment (MI) on exercise capacity and quality of life in patients with Parkinson disease (PD). One hundred ninety-two patients (≥50 years old) were divided according to the Hoehn and Yahr stages in: mild (stage I), mild to moderate (stage II), moderate (stage III), and advanced MI (stage IV). Exercise capacity (6-min walk test [6MWT]) and quality of life (Parkinson’s Disease Questionnaire [PDQ-39]) were obtained. In this context, 6MWT was progressively worse with increasing the severity of MI (P<0.01). Patients with advanced MI achieved 39% of predicted 6MWT of healthy subject, while subjects with mild MI achieved 83% of healthy subject (P<0.01). In addition, patients with advanced MI presented higher (i.e., worse) PDQ-39 scores in summary index, cognition, mobility and activities of daily live domains compared to other groups (P<0.01). Patients with moderate MI also presented worse scores in PDQ-39 summary index, mobility and activities of daily live domains in comparison with mild MI patients (P<0.01). Higher MI was correlated with worse exercise capacity (6MWT: r=−0.46, P<0.01), with worse PDQ-39 summary index and the mobility and activities of daily live domains scores (r=0.38, r=0.46, and r=0.43, P<0.01). In conclusion, MI is related to lower exercise capacity and quality of life (i.e., PDQ-39 summary index and mobility and activities of daily live domains) in patients with PD.
INTRODUCTION
In the last 25 years, the prevalence of people with Parkinson disease (PD) worldwide more than double from 2.5 million to 6.1 million (GBD 2016 Parkinson’s Disease Collaborators, 2018). PD is a progressive neurodegenerative disease characterized by motor impairment (MI), involving resting tremor, rigidity, bradykinesia, and postural instability, affecting the mobility (Dickson, 2018; Jankovic, 2008) and reduced survival in these patients (Lo et al., 2009).
The Hoehn and Yahr scale (HY) is the most common applied tool for evaluate the level of clinical disability in these patients. As an indicator of PD progression, change in HY stage (i.e., stages 1–5: mild-severe levels) is an important feature in the course of the PD (Goetz et al., 2004). In this context, previous studies (Falvo and Earhart, 2009; Ivey et al., 2012) observed relationship between worse exercise capacity (6-min walk test [6MWT]) and higher MI assessed by the HY scale in patients with mild to moderate PD (i.e., stages 1–3). Despite these results, studies including patients in more advanced stage of PD are still needed for a better understanding of this relationship.
Balzer-Geldsetzer et al. (2018) also observed relationship between higher MI assessed by the HY scale and worse global quality of life as well as in some of the domains of quality of life (i.e., mobility, activities of daily live, emotional well-being, cognition, and communication domains) in patients with mild to moderate PD. However, although previous studies (He et al., 2016; Rosqvist et al., 2021) have also observed relationship between higher MI and worse global quality of life in patients with advanced PD, they did not assess the different domains of quality of life. So, the impact of greater MI severity on the different domains of quality of life is unclear.
The gap finding regarding the role of MI severity accessed by the HY scale on exercise capacity and quality of life can be caused by limited characteristics of the sample studied (i.e., HY stages 1–3), limiting the understanding the consequences of PD on MI severity spectrum. Therefore, in the aim of the present study was to analyze in patients with PD with severity ranging from HY stage 1 to 4 the relationship between MI on exercise capacity and quality of life.
MATERIALS AND METHODS
Design
This study has a cross-sectional study performed in a single center between October 2016 and April 2019. For data analyses, patients with PD were divided according to the HY stages in: mild (stage I), mild to moderate (stage II), moderate (stage III), and advanced MI (stage IV). Sociodemographic and clinical information was obtained through a face-to-face interview. In addition, exercise capacity and quality of life were also assessed. All the evaluations were performed with patients in the “on state” of their medication of PD.
Subjects
Patients with PD were recruited from The Brazil Parkinson Association. Patients were included if they met the following criteria: age ≥50 years old; diagnosis of PD; and stages I–IV of the HY. Exclusion criteria included: presence of any health problem that preclude tests. The study was approved by the local ethical committee (CAAE: 15050713.6.2004.0065), according to the Declaration of Helsinki, and written informed consent was obtained from the patients.
Clinical evaluation
The patients’ clinical stages were assessed using the HY scale, raging I (mild problem) to stage V (advanced disease) (Goetz et al., 2004). Their IM was also assessed using the Unified Parkinson’s Disease Rating Scale (UPDRS) part III (Goetz et al., 2008). It consists of 27 items (bradikynesia, rigidity, tremor, and axial signs), ranging 0 (no problem) to 4 points (severe problem). Levodopa equivalent dose (LED) was calculated using a previously published formula (Tomlinson et al., 2010).
Exercise capacity evaluation
The 6MWT was performed along a 30-m corridor. A cone was placed at each end of the walkway to indicate where the patient had to turn. Patients were instructed to cover as much distance as possible in 6 min (ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories, 2002). Six-min total distance was defined as the maximum distance achieved by the patient at the end of the test. The percentage of predicted 6MWT of a healthy subject with similar characteristics was calculated using the procedures previously described (Iwama et al., 2009).
Quality of life
Quality of life was assessed using the validated Brazilian version of the Parkinson’s Disease Questionnaire (PDQ-39) (Carod-Artal et al., 2007). Each of its 39 questions uses the 5 points ordinal scoring system. It has eight domains: mobility, activities of daily live, emotional well-being, stigma, social support, cognition, communication, and bodily discomfort. The questions are presented below:
Mobility: 1. Had difficulty doing leisure activities? 2. Had difficulty looking after your home? 3. Had difficulty carrying shopping bags? 4. Had difficulty walking half a mile? 5. Had difficulty walking 100 yards? 6. Had difficulty getting around the house? 7. Had difficulty getting around in public places? 8. Needed to be accompanied when went out? 9. Felt frightened or worried about falling in public? 10. Been confined to the house more than liked?
Activities of daily live: 1. Had difficulty washing yourself? 2. Had difficulty dressing yourself? 3. Had problems doing up buttons or shoe laces? 4. Had problems writing clearly? 5. Had difficulty cutting up your food? 6. Had difficulty holding a drink?
Emotional well-being: 1. Felt depressed? 2. Felt isolated and lonely? 3. Felt weepy or tearful? 4. Felt angry or bitter? 5. Felt anxious? 6. Felt worried about your future?
Stigma: 1. Felt you had to conceal PD? 2. Avoided eating or drinking in public? 3. Felt embarrassed about having PD? 4. Felt worried about other people’s reaction to you?
Social support: 1. Had problems with close relationships? 2. Lacked support from your spouse or partner? 3. Lacked support from friends’ family or close friends?
Cognition: 1. Unexpectedly fallen asleep during the day? 2. Had problems with concentration? 3. Felt your memory was bad? 4. Had distressing dreams or hallucinations?
Communications: 1. Had difficulty with speech? 2. Felt unable to communicate properly? 3. Felt ignored by people?
Bodily discomfort: 1. Had muscle cramps or spasms? 2. Had aches or pains? 3. Felt unpleasantly hot or cold?
Answers for each of the questions range from 0 (never) to 4 (always). Subscale scores and a summary index representing the quality of life may also be calculated (0–100), with higher scores representing worse quality of life (Carod-Artal et al., 2007).
Statistical analyses
The chi-square was used for comparing differences among the groups regarding categorical variables. Generalized linear model was used for continuous variables. Correlation between the HY and functional capacity and the different domains of quality of life was analyzed by Partial correlation. In both analyzes, age, gender, disease duration, and LED were employed as covariate. Post hoc pairwise comparison using the Bonferroni correction for multiple comparisons was employed when necessary. All statistical analysis was performed using IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA). Significance level was defined as P≤0.05.
RESULTS
One-hundred ninety-two patients with PD were included in the study, being 26 with mild MI, 51 patients with mild to moderate MI, 92 patients with moderate MI, and 23 patients with advanced MI. Their characteristics are shown in Table 1. Groups were similar regarding body mass index, comorbidities, and medications for other comorbidities. However, patients with moderate MI presented difference for the gender proportion compared to the other patients. Patients with advanced MI were older and had longer disease duration compared to other patients. Patients with mild to moderate and moderate MI were older and had longer disease duration compared to patients with mild MI. Patients with more MI also presented higher UPDRS part III score compared to the other patients. In addition, patients with moderate and advanced MI had a higher LED compared to the other patients.

Characteristics of the patients with Parkinson disease divided according to motor impairment (n=192)
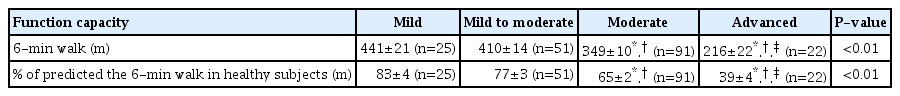
Patients with advanced MI had worse performance on 6MWT compared to other patients. Patients with moderate MI were also worse compared to patients with mild and mild to moderate MI. Patients with advanced MI achieved 39% of predicted 6MWT of a healthy subject, while subjects with moderate MI achieved 65% and subjects with mild to moderate and mild achieved 77% and 83% of a healthy subject, respectively (Table 2).
Patients with advanced MI had worse scores in PDQ-39 summary index and mobility, activities of daily live, and cognition domains compared to other groups. Patients with moderate MI also presented worse scores in mobility domain in comparison with mild and mild to moderate MI patients and worse scores in PDQ-39 summary index and activities of daily live domain in comparison with mild patients. There was no difference between patients with mild and mild to moderate MI (Table 3).

Scores corresponding the different domains of quality of life of patients with Parkinson disease divided according to motor impairment
Higher MI correlated with worse exercise capacity (6MWT: r=−0.46; % of predicted the 6MWT in healthy subjects: r=−0.47, P<0.01). In addition, except for stigma domain (r=−0.02, P≥0.05), higher MI correlated with worse scores in all other domains of quality of life (i.e., PDQ-39 summary index, r=0.38; mobility, r=0.46; activities of daily live, r=0.43; emotional well-being, r=0.17; social support, r=0.21; cognition, r=0.24; communication, r=0.30; and bodily discomfort domains, r=0.15; P≤0.05).
DISCUSSION
The main findings of the current study were that the severity of MI assessed by the HY scale is related to lower exercise capacity and quality of life (i.e., PDQ-39 summary index and mobility, activities of daily live and cognition domains) in patients with PD.
The results of the current study indicated that higher MI occurred in patients older and with longer disease duration. Aging and disease duration are independent risk factors for motor symptoms in these patients. Specifically, disease duration, this is consistent with the natural history of PD as a progressive neurodegenerative disease, where MI progress throughout the course of disease (Hattori et al., 2014). However, although the relationship between aging and MI be consensus, the mechanisms surrounding the aging process on PD are unclear (Obeso et al., 2010). It has been assumed that the aging process increases the vulnerability and loss of dopaminergic neurons to toxic insult because of increasing failure of normal cellular physiological and biochemical processes and, consequently, impairment motor control of these patients (Schapira and Jenner, 2011).
Patients with higher MI had more difficulty to complete 6MWT. In fact, HY stages were moderately correlated with worse exercise capacity. These results are in accordance with a Falvo and Earhart (2009) that also observed that higher MI is associated with lower 6MWT and with Barbieri et al. (2012) that observed association with lower 880-yd walk test performance in patients with mild to moderate disease severity. Higher HY stage reflects in a worse bradykinesia, rigidity, tremor, and instability postural (Goetz et al., 2004) and, consequently, limits the tasks evaluated during 6MWT. In fact, previous studies (Falvo and Earhart, 2009; Kobayashi et al., 2017) demonstrated that 6MWT is associated with walk speed, balance, and agility. In addition, patients with advanced MI achieved only 39% of a healthy subject, while patients with moderate MI achieved 65%, patients with mild to moderate MI achieved 77% and patients with mild MI achieved 83% of a healthy subject. These responses are similar to other diseases in which patients have major motor limitations, such as intermittent claudication and stroke (Correia et al., 2020; Pradon et al., 2013). Interestingly, the lower exercise capacity in patients with more severe MI occurred despite the higher LED use in these patients, which suggests that drug treatment is not completely effective in controlling MI from PD.
In this current study, advanced MI resulted in worse mobility, activities of daily live, and cognition domains, consequently, quality of life PDQ-39 summary index. In addition, moderate MI also resulted worse mobility, activities of daily live domains and, consequently, quality of life PDQ-39 summary index compared to patients with mild MI. In fact, HY stages were moderately correlated with worse the mobility and activities of daily live domains and, consequently, PDQ-39 summary index of quality of life. Balzer-Geldsetzer et al. (2018) also observed that moderate MI resulted worse mobility and activities of daily live domains and quality of life PDQ-39 summary index compared with patients with less MI. Higher MI results in more difficulty for patients to perform tasks related mobility (e.g., walking) and activities of daily live (e.g., dressing, eating, etc.), parameters encompassed by HY stages (i.e., bilateral involvement, postural instability, and severe disability but still able to walk or stand unassisted) (Goetz et al., 2004) obtained in this current study. Regarding cognition domains result, higher MI has been associated with reduction in the physical activity level in patients with PD (Bryant et al., 2016), contributing, consequently, with impairment on cognitive capacity (Shih et al., 2019).
The results of the current study have some practical relevance, since it was possible to observe that the severity of MI assessed by the HY scale is related to lower exercise capacity and quality of life in patients with PD. In practical terms, the HY scale is a practical and fast scale designed to assess the MI and understanding the relationship between the severity of MI and exercise capacity and quality of life may allow clinicians and others rehabilitation professionals to better quantify physical functioning and quality of life, longitudinally assess disease progression, and also assess the efficacy of interventions. Furthermore, the results emphasize the importance of optimizing treatment for patients with more advanced MI.
This study had some limitations. (a) It is a cross-sectional study and so cannot establish cause and effect; (b) Patients at the HY stage 5 were excluded of this study. Thus, results cannot be generalized to all patients with PD. However, the inclusion of these patients would not guarantee the correct execution of the tests and questionnaires applied in study due their motor and non-motor impairments; (c) Results are limited the tests and questionnaires applied in this study and may be different of other tests, which should be tested.
In conclusion, MI is related to lower exercise capacity and quality of life (i.e., PDQ-39 summary index and mobility, activities of daily live and cognition domains) in patients with PD.
ACKNOWLEDGMENTS
Fundação de Amparo à Pesquisa do Estado de São Paulo – FAPESP’ (2013/07699-0). RMR receive a research productivity fellowship granted by Brazilian National Council for Scientific and Technological Development. We gratefully acknowledge the volunteers and The Brazil Parkinson Association and the Research, Innovation and Dissemination Center for Neuromathematics (NeuroMat).
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.