Effect of regular endurance exercises on management of cardiovascular health in middle-aged men
Article information
Abstract
This study was conducted to investigate the effect of regular endurance exercises on the management of cardiovascular health in middle-aged men. The following conclusions were drawn as the result of comparatively analyzing middle-aged men who regularly performed triathlon and cycling exercises for more than 5 years. The effect of regular endurance exercises on cardiovascular health management in middle-aged men was found to be relatively positive. However, prolonged endurance exercises can cause cardiovascular disease which can adversely affect the cardiac function, and to date, no defining limit is known about the amount of exercise that improves the cardiovascular function while reducing the cardiovascular events. Therefore, aiming for exercises at moderate intensity that befit the individual’s fitness level as well as conducting regular examinations to predict and manage the risk of sudden cardiac death from exercising were considered as the more effective method of cardiovascular health management.
INTRODUCTION
Middle-aged individuals of the modern society are highly likely to be exposed to geriatric diseases, which are chronic disorders, due to their sedentary lifestyles and decrease in physical activities. In response to this, exercising has been highly recommended as a measure to prevent such diseases. In addition, regular exercise is effective for the prevention and treatment of chronic diseases such as coronary artery disease, diabetes, obesity, hypertension, cardiac failure, and depression, and reportedly extends the average lifespan of active individuals by approximately 7 years, as compared to individuals with a sedentary lifestyle (Chakravarty et al., 2008; Haskell et al., 2007).
The 2008 Physical Activity Guidelines Advisory Committee Report recommended a minimum 150 min/wk of moderate intensity or 75 min/wk of vigorous-intensity aerobic exercise for an adult. Excessive exercise above these recommendations that regularly engage over 20 hr per week at an intensity of 15 metabolic equivalent of tasks (MET) induces a plethora of unique electrical, structural, and functional cardiac adaptations that are collectively termed the ‘athlete’s heart’ (Fagard, 2003; Mann and Rosenzweig, 2012). On the other hand, while there are numerous studies which identify physical activities and exercises to be beneficial, there are also meta-analyses involving athletes engaged in chronic exercise that reported a 5-fold risk of fatal arrhythmia, like atrial fibrillation, compared with the sedentary population (Karjalainen et al., 1998), and enhanced coronary event rates (Vlachopoulos et al., 2010). In addition, it has been reported that long-term endurance exercises have the potential to adversely affect the cardiac function by inducing cardiovascular diseases, and till now, no defining limit is known about the amount of exercise that improves the cardiovascular function while reducing the cardiovascular events. Nevertheless, the popularity of athletic events and average age of participants have increased worldwide over the past 30 years, and completing in endurance events has become a personal goal for many individuals (Eijsvogels et al., 2016).
Furthermore, the main cause of sudden cardiac death among athletes under the age of 35 has been congenital heart diseases such as hypertrophic myocardiopathy; for athletes over 35 years, 70% of sudden cardiac death was induced by coronary artery diseases (Burke et al., 1992). Over the past 35 years, 135 Americans partaking triathlon died suddenly during exercise, 44% of whom died of atherosclerotic coronary artery diseases or myocardiopathy (Harris et al., 2017). As exercise-induced hypertension has been recently reported in runners, it was observed that fatal arrhythmia was closely associated with intensity and length of exercise (Kim et al., 2017). In this study, we investigated the cardiovascular effects and remodeling through graded exercise testing and echocardiography with middle-aged men who had participated in chronic excessive endurance exercise like triathlon and cycling.
MATERIALS AND METHODS
Subjects
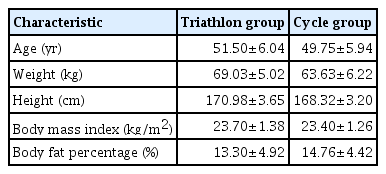
The subjects of this study were individuals living in city Seoul, partaking in triathlon (TG, n=8) and cycling (CG, n=8) exercises. The subjects had more than 5 years of experience in the exercises and were exercising 4 to 5 times a week, 1 to 2 hr per session. In terms of the exercise intensity, the study subjects had been exercising regularly at 13–15 on the rating of perceived exertion for each session. This study was approved by the Institutional Review Board of Pusan National University (PNU IRB/2015-31-HR) prior to commencement. Information on the program was provided befitting to the purpose of this study, and only the subjects who wished to participate in the experiment and provided their consent to participate in a consent form were involved in this study. The general characteristics of subjects are described in Table 1.
Measurement item and method
This study measured and analyzed the body compositions (weight, body fat percentage, body mass index), exercise stress tests (heart rate and blood pressure at rest and during exercise, electrocardiogram, cardiopulmonary fitness, myocardial ischemia, arrhythmia), and echocardiography (heart structure and function).
Echocardiography
Every subject that was prohibited from performing exercise a day before their examination, was also prohibited from consuming caffeinated drinks, alcoholic beverage, smoking, and cold medicine 12 hr before their examination. M-mode heart ultrasound waves were detected by the 5-MHz transducer of the echocardiography instrument to evaluate the structure and function of the heart. The electrocardiography measurement relied on the guidelines of the American Society of Echocardiography (Sahn et al., 1978).
The measurement items were left ventricular inter dimension at end-diastole (LVIDd), left ventricular inter dimension at end-systole (LVIDs), interventricular septal thickness end-diastole (IVSd), left ventricular posterior wall thickness at end-diastole (LVPWd), left ventricular end-diastolic volume (LVEDV), left ventricular stroke volume (LVSV), left ventricular cardiac output (LVCO), left ventricular ejection fraction (LVEF), left ventricular mass (LVM), and LVM index (LVMI). LVM was calculated using the formula:
where LVED, left ventricular end diastolic diameter; PWTd, posterior wall thickness in diastole; SWTd, septum wall thickness in diastole.
The value of LVMI was obtained by dividing with body surface area. Diastolic function was determined by the tissue pulsed Doppler with E (E-velocity, peak mitral velocity of early filling), A (A-velocity, peak atrial velocity of atrial filling), E/A ratio, E′ (E′-velocity, early diastolic annulus velocity), A′ (A′-velocity, late diastolic annulus velocity), E′/A′ ratio, E/E′ ratio, and deceleration time (DT).
Data processing
The mean and standard deviation of all measured items were calculated using IBM SPSS Statistics ver. 21.0 (IBM Co., Armonk, NY, USA), and analyzed using an independent sample t-test to test the difference of means between groups. The statistical significance level was set as α=0.05.
RESULTS
Effects on the cardiovascular factors
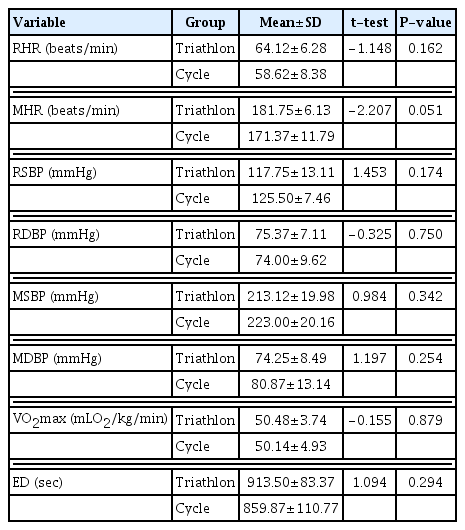
The following results were obtained from analyzing the effects of the two groups, the triathlon and cycling groups, on the cardiovascular factors (Table 2). No significant differences were identified between the two groups for the resting heart rate, maximal heart rate, resting systolic blood pressure, resting diastolic blood pressure, maximal systolic blood pressure, maximal diastolic blood pressure, maximal oxygen uptake, and the exercise duration. However, both groups showed exercise-induced hypertension in the maximal systolic blood pressure results.
Effects on the heart structure
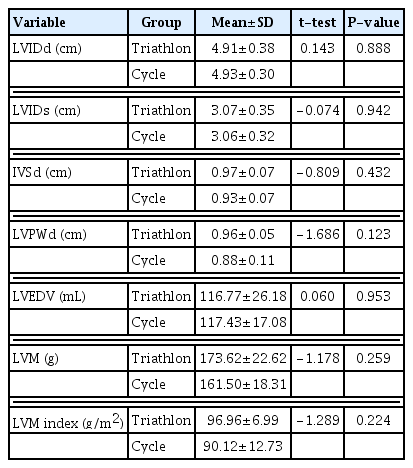
The following results were obtained on analyzing the effects of the two groups, the triathlon and cycling groups, on the heart structure (Table 3). Similar to the cardiovascular factors, no significant differences were identified between the two groups for the heart structure in the LVIDd, LVIDs, IVSd, LVPWd, LVEDV, LVM, or LVMI.
Differences in the heart function
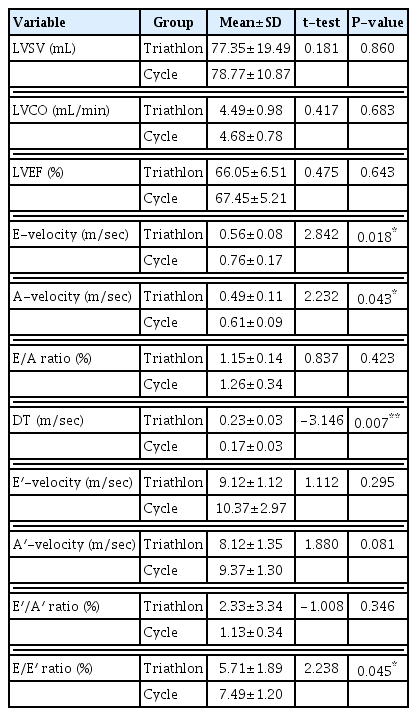
The following results were obtained from analyzing the effects of the two groups, the triathlon and cycling groups, on the cardiac function (Table 4). No differences were found between the two groups for the cardiac function in the LVSV, LVCO, LVEF, E-velocity (peak mitral velocity early filling), A-velocity (peak atrial velocity early filling), E/A ratio (ratio of peak mitral early and atrial filling velocities), or E′/A′ ratio (ratio of early diastolic annulus velocity and late diastolic annulus velocity). However, there were significant differences in the early diastolic annulus velocity (P< 0.05), late diastolic annulus velocity (P<0.05), DT (P<0.01), and the ratio of the peak mitral early and early diastolic annulus velocity (P<0.05).
DISCUSSION
In this study, exercise stress tests and echocardiography were conducted on the subjects who regularly participated in triathlon and cycling exercises, and the cardiovascular factors, heart structures, and cardiac functions were analyzed for each group. Cardiac injuries associated with sports have been discussed extensively (Leischik and Spelsberg, 2014; Oxborough et al., 2010), exercises have been observed to be particularly improving the functional status of patients with cardiac conditions in addition to providing prevention and treatment of cardiovascular diseases, and reducing the risk factors (Flynn et al., 2009; Lawler et al., 2011). However, sudden death is the leading exercise-related cardiac injury with most athletes under the age of 35 dying from coronary artery disease (Wike and Kernan, 2005), while the other general causes include hypertrophic cardiomyopathy, coronary disease, coronary anomalies, myocarditis, and arrhythmogenic right ventricle (Marijon et al., 2011; Solberg et al., 2010). Not all of the differences in the cardiovascular factors were found to be significant in this study, but both groups showed exercise-induced hypertension for the maximal systolic blood pressure.
Exercise-induced hypertension refers to systolic blood pressure and diastolic blood pressure being less than 140/90 mmHg at rest, and the systolic blood pressure reaching 210 mmHg or above at maximal exercise (Singh et al., 1999). One study reported individuals with exercise-induced hypertension to be five to ten times more likely to develop hypertension in the future (Singh et al., 1999), and exercise-induced hypertension as an independent risk factor for cardiovascular diseases (Tzemos et al., 2015). The mechanism of exercise-induced hypertension is known to be caused by the blood pressure which excessively elevates with increased exercise intensity, as the peripheral vascular resistance increases from vasodilation disorder that is caused by the dysfunction of vascular endothelial cells (Stewart et al., 2004; Wilson et al., 1990). Other studies on exercise-induced hypertension reported that it could cause eccentric remodeling of the cardiac structures in people who performed prolonged endurance training (Hoogsteen et al., 2004), as well as other remodeling processes alike (Karlstedt et al., 2012; La Gerche et al., 2012; Leischik et al., 2014). Participants of triathlon exercises may develop a temporary overload (Oomah et al., 2011), and it was also reported that the inner diameter of the left ventricle and the thickness and mass of the middle and posterior ventricular walls increased from exercising, due to the increase in the arterial pressure (Gerche et al., 2011; Leischik and Spelsberg, 2014), which are also consistent with the results of this study.
These results indicate the consequences of chronic vascular pressure caused by high exercise intensity over a prolonged period which suggest that such results may be caused by the stress that accelerates the fibrosis of various myocardium conditions (Heidbuchel et al., 2011; Vlachopoulos et al., 2010). Furthermore, the increase in the left ventricle also showed an elevation in the end-diastolic left ventricular volume, LVM, and LVMI. However, ventricular hypertrophy and high LVM identified in this study were not pathological conditions such as congenital hypertrophic cardiomyopathy, which can cause sudden death in young athletes (Maron et al., 2009), and there were no statistically significant differences in the heart structure between the two groups. On the other hand, the term ‘athlete’s heart’ (George et al., 1991) has been used since 1899 as endurance training-type exercises such as triathlon and cycling were known to physiologically induce cardiovascular adaptation and systematic changes in the cardiac structure (Utomi et al., 2014) and produce beneficial changes (McMullen et al., 2007). However, continuous follow-up investigations are needed as it was reported that structural changes in the left ventricle were associated with an increased risk of cardiovascular morbidity and mortality (Kim et al., 2020).
In terms of heart functions, the heart rate of 60 beats per minute and the diastolic blood pressure close to the state of bradycardia at rest, which are generally found in hemodynamic responses from the effect of long-term exercise, corresponded with the results of this study. Upon examining the previous studies, this phenomenon appears to have been caused by the high stroke volume and increased vagal tone from exercise adaptation (Sugiura et al., 2015). Moreover, those who performed exercises over a long period were found to have increased cardiac output of up to 40 L (Pluim et al., 2000), which might be the result of maintaining cardiac output as a compensatory mechanism for the increase in the stroke volume. However, no statistically significant effects were found in this study despite the increase in the figures, which suggests that regular and long-term performance of any type of exercise can improve the heart function.
The LVEF, an index representing the contractility of the left ventricle, is evaluated by the ratio of the total blood volume entering the left ventricle and the remaining blood volume after one ejection. A study which investigated the LVEF between exercising and nonexercising groups, as well as the differences between endurance and strength athletes, showed no significant differences between the groups (Vinereanu et al., 2002), which were also consistent with the results of this study. As the pressure in the left atrium becomes higher than that of the left ventricle, the mitral valve opens and blood flows in rapidly, which is referred to as the mitral velocity early filling stage. When the left atrium contracts, the remaining left atrial blood flows into the left ventricle, which is referred to as the peak atrial velocity early filling stage (Hurrell et al., 1997). The figures were slightly higher or lower in this study, but all the figures were within the normal ranges and were found to have a statistically significant effect.
The reason for this is that the DT and early diastolic annulus velocity were lower in the aerobic and anaerobic exercise groups as well as the triathlon athletes in comparison to the general population (Naylor et al., 2005), and the ratio of peak mitral and atrial early filling velocities have also been reported as high (Douglas et al., 1986), which was also consistent with the results of this study. In addition, athletes participating in the endurance exercises were reported to have slightly higher early diastolic annulus velocities and late diastolic annulus velocities (Vinereanu et al., 2002), but no statistically significant differences were found in the ratio of early diastolic annulus velocities and late diastolic annulus velocities (Caselli et al., 2015), which were also consistent with the results of this study. Moreover, the ratio of peak mitral early and early diastolic annulus velocity, which was considered as the normal when less than eight, and abnormal when greater than 15, was found to have a statistically significant effect on the two groups. However, one study reported the ratio of peak mitral early and early diastolic annulus velocity to be unaffected by exercise (Caselli et al., 2015). Therefore, this is considered to hold no clinical significance as the results from this study were within the normal ranges. To summarize the abovementioned results, regular endurance exercises were found to have a relatively positive effect on the management of cardiovascular health in middle-aged men.
However, studies on prolonged exercise and lifelong endurance athletes suggest that prolonged exercise training may create scarring, fibrosis, and myocardial injury even in individuals without a genetic predisposition to cardiomyopathy (Gerche et al., 2012). Therefore, aiming for exercises at a safe moderate intensity that befit the individual’s fitness level and conducting regular examinations to predict and manage the risk of sudden cardiac death from exercising were considered as the more effective methods of cardiovascular health management.
ACKNOWLEDGMENTS
The authors received no financial support for this article.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.