Assessment of the feasibility of 1-min sit-to-stand test in evaluating functional exercise capacity in interstitial lung disease patients
Article information
Abstract
Six-min walk test (6MWT) is widely used exercise test for the evaluation of interstitial lung disease (ILD). However, the long test duration and need for long and flat surface hinder its routine use. One-min sit-to-stand test (1-STST) is devoid of such limitations, but has been scarcely evaluated. The study was conducted to evaluate the performance of 1-STST by correlating it with 6MWT in ILD patients. Stable ILD patients were prospectively enrolled. After initial spirometry, all patients performed 6MWT and 1-STST following the standard recommendations. Exercise capacity and physiological parameters (heart rate, pulse oxygen saturation, blood pressure and dyspnea [modified Borg scale]) including peripheral oxygen saturation (SpO2) were correlated after the tests using Pearson correlation, Intraclass correlation coefficient (ICC) and kappa (κ) coefficient. The results showed that the mean age of the patients (n=60) was 58.8±11.5 years (male:female=1:1). Repetitions after 1-STST showed significant correlation with 6MWT (r=0.48; P<0.001). Changes in the physiological variables were similar (P>0.05) with good consistency (ICC=0.68–0.95) between 6MWT and 1-STST. Both lowest SpO2 and difference in SpO2 also showed good agreement (ICC=0.86; 95% confidence interval [CI], 0.77–0.92 and ICC=0.68; 95% CI, 0.47–0.81 respectively) and significant correlation (r=0.76 and r=0.52, respectively). 1-STST and 6MWT were consistent in identifying patients having oxygen desaturation ≥4% (κ=0.56; 96% CI, 0.30–0.82). The results demonstrated that the performance of 1-STST was consistent with 6MWT in terms of exercise capacity and change in physiological parameters. 1-STST can be a valid alternative to 6MWT in the assessment of ILD patients, especially in peripheral health centers.
INTRODUCTION
Interstitial lung disease (ILD) is a chronic lung disease characterized by interstitial inflammation and fibrosis. The disease is classified into various types based on the underlying causes. Due to varied etiology, ILD often has diverse presentations and an unpredictable course. Few ILDs like hypersensitivity pneumonitis and connective tissue disease associated ILD are treatment responsive and reversible to a variable extent, whereas, others like Idiopathic pulmonary fibrosis (IPF) have chronic progressive course. Hence, serial monitoring of the disease to assess treatment response is a vital part of disease management. Standard methods routinely used for monitoring include lung function test and arterial blood gas analysis. However, these tests are done under resting conditions and are usually normal for an extended time during the early course of disease (Bennett et al., 2015). In addition, infrastructural cost of both the tests and need for procedural training (in case of lung function study) limit their universal applicability. Exercise testing has emerged as a promising method of disease evaluation that can also be useful in early phase of the disease (ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories, 2002; Bui et al., 2017).
Out of different exercise tests, 6-min walk test (6MWT) has been extensively evaluated and validated to measure exercise tolerance in many chronic respiratory diseases like chronic obstructive pulmonary disease (COPD) (Dogra et al., 2015; Marin et al., 2001), ILD (Harari et al., 2022; Lama et al., 2003) and cystic fibrosis (López-de-Uralde-Villanueva et al., 2021). Oxygen desaturation during 6MWT is a risk factor for poor survival and mortality in patients with idiopathic interstitial pneumonia (du Bois et al., 2014; Lama et al., 2003). American Thoracic Society/European Respiratory Society guidelines recommend assessment of exercise induced desaturation as a prognostic indicator in ILD patients (Cottin et al., 2017; Raghu et al., 2011). 6MWT is easy to perform, reproducible and does not require costly infrastructure. However, it is time consuming and requires a 30-m-long corridor which is not be available in many health centers. The test is sensitive to changes in methodology such as supplemental oxygen, track layout and length and to variation in verbal instructions (Holland et al., 2015).
To overcome the limitations, 1-min sit-to-stand test (1-STST) has been evaluated in different respiratory conditions (Bohannon and Crouch, 2019). It is a field test that is less time consuming and requires only a standard chair, on which a patient is supposed to perform stand up and sit-down maneuvers as many times as possible in 1 min. The available evidence supports its use as a valuable alternative to 6MWT in COPD patients (Ozalevli et al., 2007; Reychler et al., 2018). However, studies on the use of 1-STST in ILD has been sparse with a few showing positive correlation between 1-STST and 6MWT in terms of lowest (nadir) peripheral oxygen saturation (SpO2) (Briand et al., 2018; Oishi et al., 2022). However, the results have not been uniform, with a lack of collective evaluation of all the common variables. Hence the presents study was conducted to correlate the performance of 1-STST with 6MWT as well as to compare the effect of these exercise tests on common cardiorespiratory variables in a cohort of ILD patients.
MATERIALS AND METHODS
The prospective study was conducted in a tertiary care teaching hospital from December 2020 to May 2022. All patients of stable ILD were consecutively enrolled from pulmonary outpatient department. Based on the previous evidence on the correlation between 6-min walk distance (6MWD) and 1-STST repetitions in ILD patients, a minimum sample size of 30 patients was required to achieve Pearson correlation coefficient (r) of 0.5 with 80% power and 5% level of significance (Briand et al., 2018). ILD was diagnosed based on the clinical and radiological features with or without histopathological evidence, following the standard guidelines (Crouser et al., 2020; Raghu et al., 2020; Raghu et al., 2022). Patients with respiratory comorbidities like COPD and lung cancer, those with history of acute exacerbation/respiratory infection in the preceding 3 months, unstable cardiac disease, those with significant joint/musculoskeletal or neurological disease that hindered successful performance of either of the tests and patients on long term oxygen therapy were excluded. All patients were explained about the purpose and procedure of the study. Written informed consent was obtained from them. The study was conducted after approval from the institute’s ethics committee (GMCH/IEC/2020/550/178 dated 01.04.2021).
A detailed history was collected mentioning the type and duration of symptoms, comorbidites, and smoking status. The modified Borg scale (0–10) was used to assess the level of dyspnea (Wilson and Jones, 1989). All patients underwent spirometry in which forced expiratory volume in 1 sec (FEV1), forced vital capacity (FVC) and the ratio of FEV1/FVC was measured. The test was performed on the Recorders and Medicare System (RMS) Helios 702 and RMS Helios 401 as per the latest guidelines (Graham et al., 2019; Stanojevic et al., 2022). Thereafter, the steps of performing 6MWT and 1-STST were explained to the patients. The tests were conducted in a random sequence, separated by rest period of at least 30 min.
Before the initiation of the 6MWT, baseline heart rate (HR), blood pressure (BP), SpO2, and the level of dyspnea (modified Borg scale) were assessed. The 6MWT was performed indoors, along a long, flat and straight 30 m corridor, following the international guidelines (Holland et al., 2014). The patient was asked to walk at their own pace on the track for 6 min. He/she was allowed to pause during the test, if necessary. After completion, the distance walked by the patient in 6 min and posttest physiological parameters were noted. Before the initiation of 1-min sit-to-stand test (1-STST), pretest cardiorespiratory parameters were measured as mentioned above. 1-STST was performed following the protocol described previously (Briand et al., 2018; Ozalevli et al., 2007). The patient was seated upright on the chair of standard (46 cm) height without an armrest, with knees flexed at 90° and arms held stationary. He/she was asked to perform repetitions of standing upright and then sitting down in the same position at a self-paced speed (safe and comfortable) as many times as possible for 1 min without using his/her arms for support while rising or sitting. Patient was permitted to rest during the test, if required. Thereafter. the number of complete repetitions and posttest physiological variables were recorded.
The distance covered, changes in SpO2, HR, BP, and change in the modified Borg score during 6MWT were compared with the number of sit-to-stand maneuvers and the changes in corresponding parameters during 1-STST.
Statistical analysis
Continuous variables were summarized as mean±standard deviation and categorical as number (percentage). Unpaired t-test was used to compare nadir and delta SpO2, peak HR, BP, and Borg scores between 6MWT and 1-STST. Ther relation between 6MWD and 1-STST repetitions as well as the relation between the physiological variables in the two tests were evaluated by Pearson correlation coefficient. Intraclass correlation coefficient (ICC) was calculated to assess agreement between nadir SpO2, change in SpO2 and HR. Agreement between the ability of the two tests to detect desaturation ≥4% was assessed using Cohen kappa coefficient (κ) with 95% confidence interval (CI). κ values of <0, 0–0.20, 0.21–0.40, 0.41–0.60, 0.61–0.80, and 0.81–1.0 were considered to indicate no, slight, fair, moderate, substantial, and almost perfect agreement, respectively. (Landis and Koch, 1977) All statistical calculations were done using IBM SPSS Statistics ver. 21.0 (IBM Co., Armonk, NY, USA). Two-tailed P<0.05 was considered significant for all statistical analysis.
RESULTS
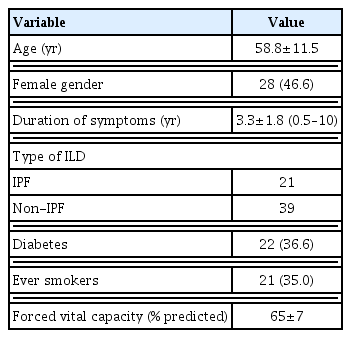
A total of 60 stable ILD patients were enrolled in the study. The mean age was 58.8±11.5 years (male:female ratio=1:1). IPF was the most common type of ILD (n=21) followed by connective tissue disease associated ILD (n=16) and hypersensitivity pneumonitis (n=11). The mean FVC and FEV1/FVC of the patients were 65%±7% and 81%±9% respectively (Table 1). Forty patients in the study cohort had FVC<70% predicted. Relation between 6MWD and 1-STST repetitions. The mean 6MWD traveled by the patients was 332±67 meters. Out of 60 patients, 50 performed the test without any halt. The mean 1-STST repetitions were 23.0±3.5 with 14 patients had 1–2 halts in between the procedure. There was moderate degree of positive correlation between the 6MWD and 1-STST repetitions (r=0.48; P<0.001) (Fig. 1). Both 6MWD and 1-STST repetitions also showed statistically significant correlation with FVC (r=0.33; P=0.01; 1-STS test r=0.45; P=0.001).
Scatter plot showing correlation between 6MWD and 1-STST repetitions. 6MWD, 6-min walk distance; 1-STST, 1-min sit-to-stand test.
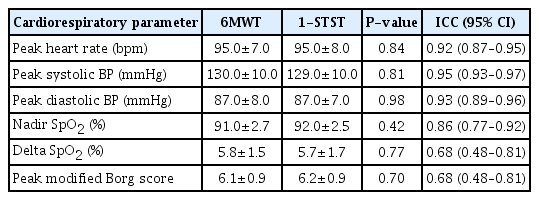
Effect of exercise tests (6MWT and 1-STST) on cardiorespiratory parameters
There was significant change in all the six physiological parameters after both 6MWT and 1-STST. The changes in all the variables after 6MWT was statistically similar to 1-STST (P>0.05) (Table 2).
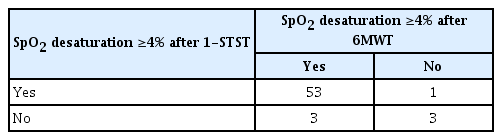
The change in SpO2 showed positive correlation (r=0.52, P< 0.001) as well as good agreement (ICC=0.68; 95% CI, 0.47–0.81; P<0.001) between 6MWT and 1-STST. Both the tests also showed moderate degree of agreement in their ability to detect oxygen desaturation ≥4% with k coefficient of 0.56 (95% CI, 0.30–0.82; P<0.001) (Table 3). Also, the nadir SpO2 values during the tests were positively correlated (r=0.76, P<0.001) with good degree of agreement (ICC=0.86; 95% CI, 0.77–0.92; P<0.001) (Fig. 2).
DISCUSSION
The present study evaluated 1-STST with 6MWT in the assessment of functional exercise capacity in ILD patients. The results showed a moderate degree of correlation between the distance covered in 6MWT and repetitions in 1-STST (r=0.48, P<0.001). The changes in cardio-pulmonary variables were also statistically similar between 6MWT and 1-STST.
6MWT is the most widely used investigation for assessing exercise tolerance in ILD patients. In the present study, distance walked by the patients during 6MWT was 332.4±67.0 m. This was similar to earlier studies by Devani et al. (2019) and Gupta et al. (2021) but other studies yielded higher values of 6MWD (Fedi et al., 2021; Tremblay Labrecque et al., 2020). This difference could be due to variations in the body stature as well as due to difference in the extent of ILD in the mentioned studies. On the other hand, number of repetitions in 1-STST was comparable to previous studies (Oishi et al., 2022; Briand et al., 2018; Tremblay Labrecque et al., 2020). On comparing, a moderate degree of correlation (r=0.48, P<0.001) was seen between 6MWD and number of 1-STST repetitions. This was in coherence with a previous work by Briand et al. (2018) that also yielded moderate correlation (r=0.50, P<0.001) between the two exercise modalities. In contrast, a stronger correlation ranging from 0.72–0.82 was seen in other studies, but the results could have been affected by small sample size (n=15 and 33) in these studies (Fedi et al., 2021; Tremblay Labrecque et al., 2020).
SpO2 is an important physiological variable measured during exercise tests. It carries high prognostic importance in different ILDs and is predictor of mortality in IPF patients (Imamura et al., 2023; Lama et al., 2003; Trushenko et al., 2023). In the present study, nadir SpO2 during 6MWT and 1-STST showed good agreement (ICC=0.86; 0.77–0.92) and a strong correlation (r=0.76, P<0.001). The results validate the previous studies that also showed good agreement (ICC=0.75–0.9) and positive correlation (r= 0.8–0.9) between the two SpO2 values (Briand et al., 2018; Oishi et al., 2022; Tremblay Labrecque et al., 2020). Likewise, delta SpO2 also showed good agreement in the study, similar to the study by Fedi et al. (2021). Fifty-six subjects (93.3%) were consistently grouped by both 6MWT and 1-STST based on oxygen desaturation of ≥4% or less, (κ=0.56; 95% CI, 0.30–0.82). Previous studies also showed a similar trend but with a higher degree of agreement (0.68–0.82) (Briand et al., 2018; Oishi et al., 2022; Tremblay Labrecque et al., 2020). The above results strongly suggest that both 6MWT and 1-STST are equally reliable in detecting changes in SpO2 in ILD patients.
In contrast to the concordance seen in SpO2, few studies suggested that 1-STST generate lower cardiorespiratory response as compared to 6MWT. As a result, nadir SpO2 and HR were found to be higher after 1-STST as compared to 6MWT in these studies (Fedi et al., 2021; Tremblay Labrecque et al., 2020). Shorter duration of 1-STST seems to be a major determinant for the lower cardiorespiratory stress generated during the test. However, the logic may not be true as similar results were not seen uniformly in other studies (Briand et al., 2018) including the present one. Moreover, the results of these studies may also not be comparable due to difference in sample size, patient population and method to measure exercise capacity.
FVC is the gold standard parameter that measures the extent of restrictive defect in ILD. In the present study, FVC showed moderate degree of positive correlation with both 6MWT (r=0.33) and 1-STST (r=0.45). However, contrary to the available evidence (Briand et al., 2018; Oishi et al., 2023), delta SpO2 and lowest SpO2 did not show any association in either of the tests. This discordance could be due to higher number of patients (66%) with poor lung function (FVC<70% predicted) in the present study as compared to 23.4% and 38.8% in studies by Briand et al. (2018) and Oishi et al. (2023), respectively. Moreover, oxygen saturation depends not only on the extent of restrictive defect (as measured by FVC) by also on the integrity of alveolar-capillary membrane and pulmonary vasculature that may affect its correlation with the FVC (Johannson et al., 2017).
Besides oxygen saturation and HR, dyspnea grade (modified Borg scale) and BP also showed similar changes after both exercise tests (Table 2). The results are in coherence with previous studies that also yielded similar findings in in terms of Borg dyspnea score (Fedi et al., 2021; Tremblay Labrecque et al., 2020) and BP (Tremblay Labrecque et al., 2020).
The present study gave a clear insight on the performance of 1-STST by comparing all common cardiorespiratory variables with those of 6MWT in ILD patients. However, there were few limitations, as well. In view of limited number of individual ILDs, subgroup analysis could not be done. However, the strength of association in the whole population was strong enough to predict the same relation in the individual ILDs. Control group of healthy subjects was not required as a part of study design, nevertheless, its inclusion could have given a better comparative picture among the three groups. A previous study by Tremblay Labrecque et al. (2020) has shown that 1-STST has a shorter learning curve, that means that after initial familiarization, a single 1-STST is sufficient to provide an accurate assessment of the exercise capacity. However, our study was not designed to evaluate such question. Lastly, this study did not involve serial measurements of 6-min walk distance or 1-STST repetitions, hence, any inference on the prognostic value of these tests could not be drawn from the available data.
The results of the present study validate the previous evidence and suggest that 1-STST can be used in place of 6MWT for evaluation of exercise capacity in ILD patients. In view of lesser infrastructural and space requirements, 1-STST may be preferred in low income as well as primary health care settings. The results also give direction for further studies with large sample and including follow-ups using serial exercise tests, that may add new dimensions to the role of 1-STST in ILD.
ACKNOWLEDGMENTS
The authors received no financial support for this article.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.