INTRODUCTION
Body weight is determined by the interaction of genetic environmental and psychosocial factors acting through the physiological mediators of energy intake and consumption (Beynon, 2023; Gao et al., 2022). Obesity is also characterized by excessively high body fat or fat tissue. In addition, life style’s changes, specially changes in diet habit, exercise, and physical activity, are considered the cornerstone of obesity management (Price and Sumithran, 2022). However, it is difficult for people who are overweight to lose weight and increase physical activity.
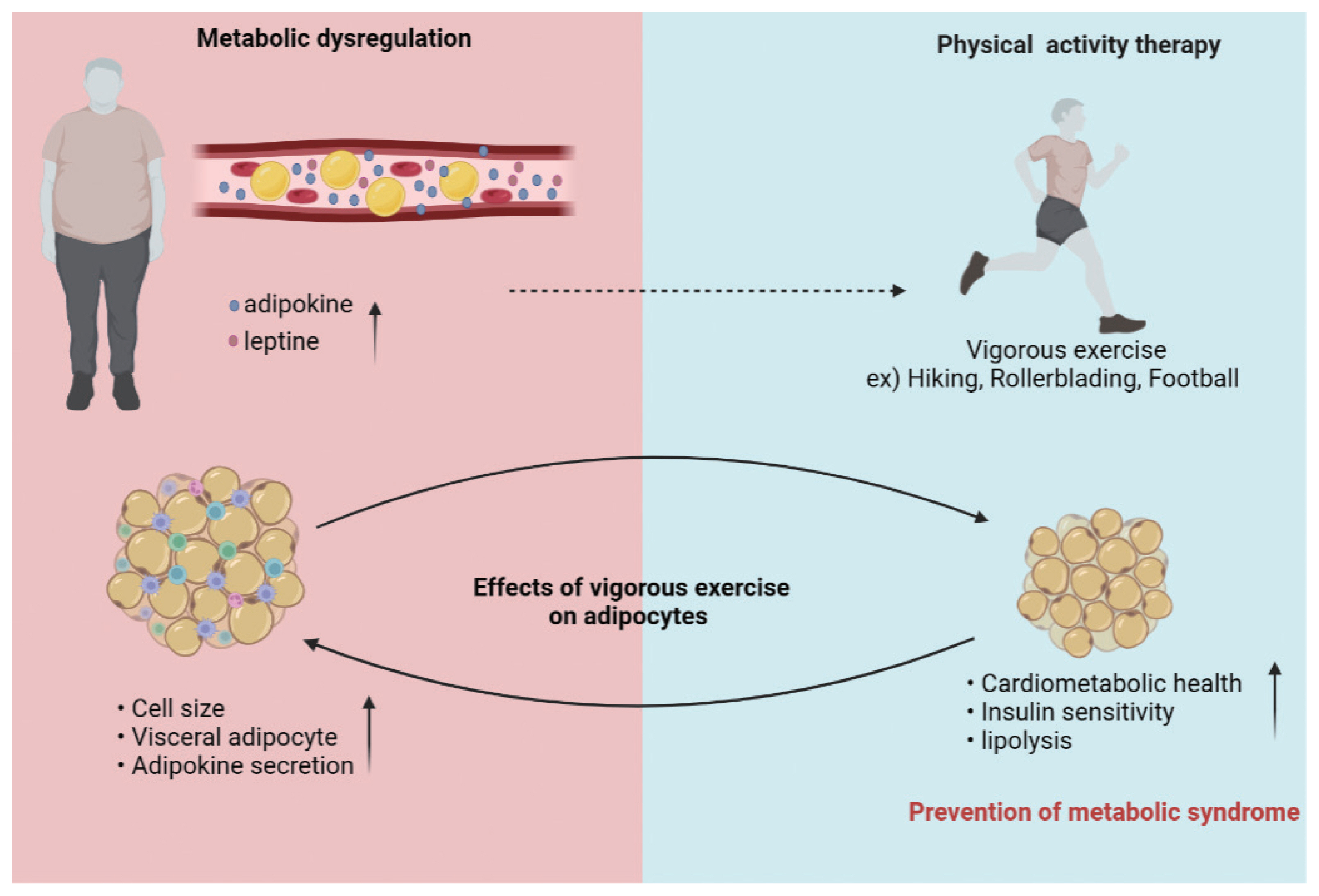
Metabolic dysregulation is a lifelong condition that requires lifestyle changes (Strasser, 2013). Most clinical recommendations for obesity treatment are based on a combination of multiple interventions, such as changes in eating habits or physical activity (Cao et al., 2023). Physical activity refers to all movements made by skeletal muscles that consume energy (Powell et al., 2011). Exercise improves the efficiency and capacity of the cardiopulmonary system and muscle strength related to health and functional capacity (Powell et al., 2011). Therefore, preventing weight gain will be more effective in reducing obesity rates than losing weight. Exercise can reduce the risks for developing obesity and metabolic dysregulation. Exercise is effective in regulating metabolism as a result of metabolic adaptation as well as strengthening skeletal muscle (Barros et al., 2022). Accordingly, major organization such as the International Association of Obesity and the American Society of Sports Medicine continue to support the need for 150 to 250 minutes of moderate-intensity physical activity per week to prevent weight gain (Armstrong et al., 2022). Some studies suggest that reduced energy intake and/or aerobic exercise are associated with reduced visceral adipose tissue (Armstrong et al., 2022; Sabag et al., 2017).
Here we outline the role of exercise on adipokines and explore their impact on the development of metabolic disorders and cardiovascular disease (CVD) in obesity. A comprehensive understanding of the mechanisms involved in the development of obesity-induced metabolic and vascular dysfunction is required for effective and tailored obesity treatment approaches.
WHAT IS THE DEFINITION OF OVERWEIGHT AND OBESITY?
Obesity has nearly tripled worldwide since 1975. Overweight and obesity are defined as excess fat accumulation or abnormal body weight. The root cause of overweight and obesity is an energy imbalance between calories consumed and calories expended. Table 1 shows the defined overweight and obesity. An increase in body mass index (BMI) increases the risk of metabolic disorders. Obese children are more likely to be obese, and obese children have an increased risk of bone fractures, high blood pressure, diabetes, and CVD. These children are exposed to high-fat, high-sugar, and high-salt diets that lead to adult obesity. Excess fat rather than overweight is associated with obesity-related diseases (Ramsay et al., 2006). Obesity is associated with many diseases, including CVD, hyperlipidemia, hypertension, endogenous diabetes, and many cancers. It has been suggested that preventing weight gain may reduce the risk of several types of cancers (Bianchini et al., 2002).
METABOLIC DYSREGULATION AND HEALTH PROBLEMS
Metabolic dysregulation is a collection of conditions that occur together and increase the risk of heart disease and stroke. This condition increases blood pressure, high blood sugar, and abnormal cholesterol or body fat around the waist. Metabolic dysregulation is closely related to overweight or obesity and inactivity. A lifelong commitment to a healthy lifestyle to prevent metabolic syndrome can prevent conditions that cause metabolic dysregulation. Disturbances in fatty acid metabolism can lead to lipid accumulation and lipotoxicity. Obesity increases the prevalence of comorbidities such as fatty liver disease, insulin-resistant type 2 diabetes, nonalcoholic fatty hepatitis, psychiatric disorders, hypertension, CVD, autoimmune diseases and some cancers.
Psychiatry disease
Several community surveys in the United States and Canada have found associations between obesity and depressive symptoms (Heo et al., 2006; Simon et al., 2006). Depression is also an important cause of suicide (Blasco et al., 2020). A relationship between depression and obesity has been reported in children and adolescents (Anderson et al., 2007). A prospective study predicted that adolescent females affected by obesity would have an increased (nearly 4-fold) risk of major depression. Several studies have reported that between 20 and 60% of obese people have a mental illness (Ramsay et al., 2006; Sarwer and Polonsky, 2016). Chronic stress in people with depression and anxiety leads to dysregulation of the hypothalamic-pituitary-adrenal axis, which increases cortisol levels associated with obesity and depression (Misiak et al., 2020). Inflammatory markers can also be found in obese and depressed people (Guest et al., 2011; Spencer and Tilbrook, 2002). One study showed that obese people have low self-esteem due to body image, which can lead to depression and anxiety (Kushner and Ryan, 2014). A Swedish study also found that obese patients suffered from depression (Rao et al., 2020). Limited epidemiological data address the relationship between obesity and anxiety. Alcohol abuse is associated with a high risk of overweight and obesity (John et al., 2005). Metabolic dysregulation may therefore explain susceptibility to psychiatric disorders.
Cancer
Overweight and obesity are associated with mortality from liver cancer, pancreatic cancer, non-Hodgkin’s lymphoma and myeloma (Calle et al., 2003). Obese adults have a higher risk of cancer than those of a healthy weight. Previous studies have reported that obesity accounts for approximately 14% of male cancer deaths and up to 20% of female cancer deaths over the past 25 years (Calle et al., 2003; Wolin et al., 2010). Obesity in postmenopausal women is directly related to circulating estradiol levels and breast cancer risk (Key et al., 2003; Missmer et al., 2004). Enhanced metabolic substrates released by altered adipose tissue play a role in tumor cell proliferation, invasion and metastasis (Kim and Scherer, 2021). Hyperlipidemia increases levels of cholesterol and non-esterified fatty acids responsible for activation of oncogenic signaling pathways, membrane synthesis and adenosine triphosphate (Samuel et al., 2018). Several studies have found that serum adiponectin levels are inversely proportional to the risk of developing several types of cancer (Miyoshi et al., 2003; Ye et al., 2014). Adipocyte/cancer cell confusion within the tumor microenvironment further leads to morphological and functional changes in both cell types, which are increasingly recognized as an integral part of cancer development and progression (Kim and Scherer, 2021). Altered fatty acid secretion and metabolism, extracellular matrix remodeling, protein and sex hormone secretion, immune dysregulation, chronic inflammation, and changes in the gut microbiome have been implicated in carcinogenesis, metastasis development, and cancer progression in obesity (Kim and Scherer, 2021; Liu et al., 2021).
Reproduction
Infertility due to masculine factors is also associated with overweight and obesity. Metabolic changes in obesity may also affect reproduction. Hypothyroidism results from central hyperleptinemia or altered hypothalamic gonadotropin releasing hormones secretion in overweight or obese patients (Chan and Mantzoros, 2001). Obesity is associated with an increased incidence of impaired ovulation and idiopathic infertility in women (Pan et al., 2023). Compared to normal-weight women, obese women may have reduced clinical pregnancy and live birth rates with increased abortion rates (Pan et al., 2023). Obese pregnant women have higher rates of maternal and fetal complications such as gestational diabetes and hypertension (Provost et al., 2016). Male obesity is also associated with reduced rates of pregnancy and fertility (Campbell et al., 2015). Some other studies have shown a correlation between increased obesity and changes in sperm parameters (MacDonald et al., 2010). Therefore, obesity is believed to play an important role in reducing fertility.
Relation of metabolic and vascular dysfunction
Adipose tissue is one of the endocrine organs of the body and is mainly composed of adipocytes capable of secreting various cellular cytokine signals known as adipokines (Atawia et al., 2019; Lehr et al., 2012). A major function of adipose or adipose tissue is energy homeostasis. Adipose tissue stores excess glucose and fatty acids through the process of adipogenesis (Choe et al., 2016). Healthy fat cells are insulin sensitive and can maintain normal blood sugar levels (Newsholme et al., 2014). Vascular pathology and dysfunction in obesity-related metabolic disorders occur through inflammatory processes (Gozal et al., 2017). This further increases levels of inflammatory signaling factors that trigger the inflammatory cycle (Atawia et al., 2019). Leptin production is regulated by inflammatory stimuli, including lipopolysaccharide, tumor necrosis factor-α, interleukin (IL)-6 and IL-1β, and plasma leptin levels increase during acute infection and inflammation (Poetsch et al., 2020). Activation of these chronic inflammatory signals in adipose tissue can promote infiltration of proinflammatory reactive oxygen species (ROS)-producing macrophages (Fernández-Sánchez et al., 2011). Obesity is associated with depleted or reduced activity of antioxidant defense enzymes such as superoxide glutathione peroxidase, catalase, and demutase (Fernández-Sánchez et al., 2011). Changes in ROS concentrations are important for cellular defense homeostasis and contribute to protective immune responses (Leloup et al., 2009; Loh et al., 2009). Accumulation of ROS can trigger maladaptive responses in metabolic dysfunction and inflammation. Inflammation is an essential immune response to maintain tissue homeostasis.
Leptin is considered a proinflammatory adipokine and leptin induces ROS production. Leptin enhances glucose utilization and insulin sensitivity under normal conditions. Hyperleptinemia is present in the clinical setting and exogenous leptin administration does not result in weight loss (Dong and Ren, 2014; Oral et al., 2002). Elevated leptin levels are associated with hypertension due to chronic activation of the sympathetic nervous system (Allison et al., 2013; Zeng et al., 2014). Circular leptin levels (>16 ng/mL) reflect the amount of energy stored in adipose tissue. It is mainly produced by fat cells and released from vesicles. Leptin also appears to play a greater role at the cardiac level, as elevated levels of circulating leptin are associated with left ventricular hypertrophy in simple obese patients (Perego et al., 2005). Increased blood volume in obese patients increases cardiac output and stimulates biomechanical stress and structural remodeling that can lead to cardiac hypertrophy (Kang et al., 2020). A correlation between cardiac hypertrophy and plasma leptin levels has been well demonstrated.
DIET STRATEGIES FOR A HEALTHY WEIGHT
Childhood obesity can be defined as the excessive accumulation of body fat in adipose tissue, which adversely affects adult health (Paes et al., 2015). Childhood obesity is the most important known risk factor for CVD in adulthood, so it needs to be managed from the beginning of life, especially in relation to lifestyle observed during this period. The Centers for Disease Control and Prevention lists a variety of colors on plates. Dark, leafy greens, oranges, tomatoes and blueberries contain vitamins, fiber and rich minerals. More important information is that it is low in added sugars, sodium, saturated fat, trans fat and cholesterol. According to one study, soy yogurt is gaining popularity as a vegan food produced simply by fermenting soy milk through proper microbial manipulation (Weng et al., 2023). Soybeans, which are rich in isoflavones, help improve hyperglycemic disorders (Weng et al., 2023). According to the Dietary Guidelines for Americans, a healthy diet includes a variety of seafood, eggs, peas, beans, nuts, seeds, fruits, vegetables, whole grains, and low-fat milk and dairy products. The most important thing to maintain a healthy weight is to recommend your daily calorie allowance.
PHYSICAL ACTIVITY TO PREVENT METABOLIC DYSREGULATION
Physical exercise has been used as an important tool for the prevention and treatment of overweight and obesity (Calcaterra et al., 2022). Moderate or high-intensity physical activity downregulates inflammatory biomarkers circulating among children (Paes et al., 2015). Although physical exercise is recommended in the adult population to combat obesity, the amount, intensity and frequency of physical activity are still controversial in the pediatric population (Paes et al., 2015). Most clinical recommendations for obesity treatment are based on a combination of several interventions, such as dietary changes, medication use, and regular physical activity (Booth et al., 2017). Current National Health Service guidelines specify ‘at least 150 min of moderate aerobic activity or 75 min of vigorous aerobic activity per week’. There is a linear relationship between energy expenditure and exercise intensity (Kim et al., 2023). People need to exercise about twice as long at light- moderate intensity to burn the same number of calories as at very intense intensity (Kim et al., 2023). The enhancing activity helps regulate blood sugar and fatty acid oxidation. Repetitive, moderate exercise has been shown to enhance the ability of skeletal muscle to absorb glucose (Egan and Zierath, 2013).
Exercise is a powerful tool to prevent metabolic disease and improve the metabolic phenotype of skeletal muscle, liver, adipose tissue and pancreas (Chow et al., 2022).
Physical exercise and increase in weight and belly fat
Low levels of physical activity consistently and independently predicted abdominal fat growth in normal-weight, overweight, and obese people (Jakicic et al., 2019). In a prospective cohort study, reported overweight was highly correlated with waist circumference and waist size (Spencer et al., 2002). Regular aerobic exercise slightly reduces waist circumference and associated visceral adipose tissue, whereas high-intensity exercise may provide superior benefits for moderate intensity (Armstrong et al., 2022). Exercise participation among middle-aged United States women was associated with a 0.10-cm reduction in waist circumference after 3 years (Sternfeld et al., 2004). Increasing physical activity regardless of weight change may be a useful strategy for preventing metabolic and other chronic diseases (Ekelund et al., 2011).
In conclusion, higher levels of physical activity consistently predicted lower waist circumferences in normal-weight, overweight and obese individuals, regardless of baseline and concomitant weight changes. Overall, physical activity is a useful strategy for preventing metabolic and other chronic diseases and premature death through its effects on central adiposity. Table 2 shows examples of moderate- and high-intensity activity for healthy adults.
Regular exercise and lipids
Regular exercise can help improve lipid disorders, including weight loss, blood pressure loss, high-density lipoprotein cholesterol (HDL)-C elevation, and triglyceride reduction (Pucci et al., 2017). One of the most obvious effects of regular exercise is its effect on insulin resistance (Roberts et al., 2013). Thune et al. (1998) studied 5,220 men and 5,869 women. BMI and detailed lipid profiles were determined at both assessments. There was a dose-response relationship between improved serum lipid levels, BMI and high levels of physical activity. Higher levels of physical activity, either through observational studies or as part of formal exercise intervention trials, generally have favorable effects on metabolic syndrome. A number of studies focusing on the relationship between aerobic exercise and HDL-C have found that HDL-C levels are more sensitive to aerobic exercise than triglyceride and low-density lipoprotein-cholesterol (LDL)-C (Couillard et al., 2001; Sirtori et al., 2019). High-level physical activity is defined as any form of physical activity that increases heart rate and respiratory rate to meet the oxygen requirements of active muscles (Pedersen and Saltin, 2006). These results suggest that exercise duration and exercise intensity all affect exercise-induced changes in blood lipids. To further lower LDL-C and triglyceride levels, higher levels of exercise intensity are required.
CONCLUSION
An increase in BMI increases the risk of metabolic disorders. Physical activity is a useful strategy to prevent death from metabolic disorders and chronic diseases. The duration and intensity of exercise have a great influence on changes in blood lipids. Lifestyle changes, especially changes in physical activity, can be said to be the cornerstone of normal-weight management (Fig. 1).